- Enroll Now - Medicare Advantage by Doc and Zip
- Health Exam Guide
- AHIP
- AHIP EXAM 50 FLASHCARDS
- 2024 - Medicare Fraud, Waste, & Abuse
- 2024 - Nondiscrimination
- 2024 - General Compliance
- Medicare Enrollment Periods
- Request a Call Back from Rachael
- Hi! I'm Rachael Kathleen Rawlins, your Insurance Agent and Retirement Planner.
- Enroll in a Medicare Plan
- Rachael's Dashboard
- I'm your MO & AR Medicare Insurance Agent. Question? Ask me.
- Book an Appointment
- Forex Trading
- AHIP 2025
- Nondescrimination
- General Compliance Training
- Medicare Cheat Sheet
- I am licensed in AR, MO, NY, OH, WV, VA, FL, TX, SC
- Health Exam Guide
- Enroll Now - Medicare Advantage by Doc and Zip
- Health Exam Guide
- AHIP
- AHIP EXAM 50 FLASHCARDS
- 2024 - Medicare Fraud, Waste, & Abuse
- 2024 - Nondiscrimination
- 2024 - General Compliance
- Medicare Enrollment Periods
- Request a Call Back from Rachael
- Hi! I'm Rachael Kathleen Rawlins, your Insurance Agent and Retirement Planner.
- Enroll in a Medicare Plan
- Rachael's Dashboard
- I'm your MO & AR Medicare Insurance Agent. Question? Ask me.
- Book an Appointment
- Forex Trading
- AHIP 2025
- Nondescrimination
- General Compliance Training
- Medicare Cheat Sheet

Rachael Rawlins
- Key Facts
- Glossary
- General Insurance
- Accident & Health Insurance Basics
- Individual Accident & Health Insurance Policy Provisions
- Disability Income and Related Insurance
- Medical Plans
- Group Health Insurance
- Specialized Health Insurance for Qualified Individuals
- Federal Tax Considerations for Accident and Health Insurance
- Arkansas Statutes, Rules & Regulations for Life & Health
- Arkansas Statutes, Rules & Regulations pertinent to Health Only
-
Key Facts
Key Facts for Arkansas Health Insurance2-50 Employees- Small Employer
2 Types of Plans - Small Employer
30+ Hours Full Time Employee
- Maternity benefits:
- 48 hours for vaginal delivery; 96 hours for cesarean section
48 Hours vaginal delivery notification
96 Hours Cesarean delivery notification
Health care insurers may not restrict a hospital stay for the mother and a newborn child to less than 48 hours for a vaginal delivery and 96 hours for a cesarean section.
1-45 Days reinstated when the company says or after 45 days, whichever comes first.
5 Days coverage for newborn infants must include routing nursery care and pediatric costs for a well newborn child for up to 5 full days in a hospital nursery or until the mother is discharged from the hospital, whichever is the shorter period.
10 Days Reinstatement probationary period starts for sickness only
14 Days Policies providing convalescent or extended care benefits following hospitalization cannot condition those benefits upon being admitted to the convalescent facility within 14 days of being discharged from the hospital.
Health Grace Period for payments - (7 days for weekly premium policies, 10 days for monthly premium policies and 31 days for all other policies)
30 Days to give back and be refunded for a medicare supplement policy.
60 Days legal actions provision before a client can sue
60 Days time payment of claims provision (so they can investigate the claim)
*** conflicting
Benefits must be payable immediately upon receipt of proof of loss and benefits for loss of time must be payable within 30 days of the period for which the insurer is liable
60 Days If the Commissioner does not disapprove the HMO's actions within 60 days of filing, the exercise of power is approved.
60 Days The Commissioner must approve or deny an application for underwriting restrictions within 60 days.
3 Months COBRA - Continuation of coverage is available only to individuals who have been insured continuously under the group policy in the 3 months before the event that terminated coverage.
Individuals must request continuation of coverage in writing no later than 10 days
90 Days Notification of the birth of the newborn child and payment of the required premium must be furnished to the insurance company within 90 days after the date of birth.
90 Days If an insurer elects to discontinue offering a particular health benefit plan, it must provide notice of discontinuation to all affected insureds at least 90 calendar days prior to the date the health benefit plan will be discontinued by the carrier.
90 Days Provide proof of loss
20 Days Provide notice of loss
90 days probationary period for health insurance coverage
180 Days If an insurer elects to nonrenew all of its health benefit plans, the insurer is required to provide advance notice of its decision to the Commissioner and all affected insureds at least 180 calendar days prior to nonrenewal
6 Months
- Pre-existing condition exclusion: no longer than 6 months
6 Months Medicare supplement policy or certificate may not exclude or limit benefits for losses incurred more than 6 months from the effective date of coverage because it involved a pre-existing condition. The policy cannot define a pre-existing condition more restrictively than a condition for which medical advice was given or treatment was recommended by or received from a physician within 6 months before the effective date of coverage.
12 months Probationary Period Max
2 Years HMOs that have been in operation for at least 2 years may offer an annual open enrollment period of at least 1 month.
24 Months Each policy must provide a minimum benefit of $6,000 for each 24-month period, no more than half of which can be spent during any period of 30 consecutive days. Each recipient of these benefits is limited to a minimum lifetime amount of $12,000.
2 Years Incontestibility Provision / time limit on certain defenses clause
5 Years If an insurer elects to nonrenew all of its health benefit plans, the insurer is required to provide advance notice of its decision to the Commissioner and all affected insureds at least 180 calendar days prior to nonrenewal
- Time limit on certain defenses — After a policy has been in force for 3 years, no misstatements, except fraudulent misstatements, made by the applicant, can be used to void the policy or to deny a claim.
3 Years To file loss and make a claim (maximum)
100 min members in operation for min 2 years for blanket coverage
(7 days for weekly premium policies, 10 days for monthly premium policies and 31 days for all other policies)
Short-Term Disability Insurance – A group or individual policy that covers disabilities of 13 to 26 weeks, and in some cases for a period of up to two years.
Group - Continuation of coverage may only be made available to individuals who have been continuously insured for 3 months prior to termination or change in marital status. An individual who wishes to continue coverage must request continuation in writing no later than 10 days after the terminating event and pay the required premium on a monthly basis and in advance.
An individual must apply for conversion no later than 30 days after termination of group coverage.
Coverage must end at the earliest of
- 120 days after continuation of coverage began
Terminally Ill – In most states, this is defined as a patient who is expected to die within 6 months of a specific illness or sickness.
- Substance abuse:
- $6,000 for each 24-month period; $12,000 lifetime minimum
- Time limit on certain defenses: 3 years
- Grace period:
- 7 days for weekly premiums
- 10 days for monthly premiums
- 31 days for any other premium mode
- Reinstatement: immediate coverage for accidents; 10-day waiting period for sickness
- Notice of claim: 20 days
- Claim forms: insurer furnishes within 15 days of notice of claim
- Proof of loss: written proof within 90 days after the end of the period for which the insurer is liable
- Payment of claims: immediately upon receipt of written proof of death
- Legal action: after 60 days but not later than 3 years after proof of loss
Key Facts A. General Insurance Key Concepts:
- Insurance is defined as the transfer of PURE risk to the insurance company in consideration for a premium.
- The chance of loss without any chance of gain is called pure risk.
- Speculative risk has the possibility for gain or loss and is not insurable.
- Risk is defined as the chance of loss.
- A condition that could result in a loss is known as an exposure.
- A hazard is something that increases the chance of loss.
- The presence of a physical hazard increases the chance of a loss occurring.
- A peril is defined as a cause of loss, such as fire.
- To be insurable, losses must be calculable.
- The law of large numbers allows insurers to predict claims more accurately.
- The law of large numbers applies to groups of people, not to individuals. The more people in the group, the more accurate the predictions are.
- Most insurers buy reinsurance to protect themselves in the event of a catastrophic loss.
- Insurance laws are not required to be uniform from one state to another.
Insurers:
- A stock insurer may pay dividends to its shareholders (stockholders), but they may not be guaranteed.
- A reciprocal insurance company is managed by an attorney-in-fact.
- An unincorporated association of individuals who insure each other is known as a reciprocal insurer.
- The government offers insurance primarily based upon social needs, such as flood insurance and workers compensation, but does not offer insurance for the purpose of preventing fraud.
- A foreign company has their home office in another state.
- An insurer incorporated outside of the U.S. who sells in the U.S. is an alien company.
Producers and General Rules of Agency:
- A producer may be personally liable when violating the producer's contract.
- Producers represent the insurance company, not the insured.
- Independent producers own their own accounts and are not insurance company employees.
- Producers have express, implied and apparent authority.
- The authority a producer has that is written in his or her contract is known as express authority.
- A producer's binding authority (if any) is expressed (written down) in the producer's contract with the insurer the producer represents.
- The authority not expressly (written) granted, but is actual authority the producer has to transact normal business activities, is known as implied authority.
Contracts:
- The elements of a legal contract may be remembered by the acronym C-O-A-L (consideration, offer, acceptance, legal purpose, and legal capacity).
- A requirement for a valid contract is offer and acceptance, or mutual agreement.
- Advertising the availability of insurance is not considered to be an offer.
- A specific and definite proposal to enter into a contract is known as an offer.
- The consideration on a policy need not be equal.
- A policy may not be voided due to unequal consideration.
- Under the consideration clause, something of value must be exchanged.
- Because insurance contracts are contracts of adhesion, policy ambiguities always favor the insured.
- Insurance policies are unilateral contracts because only one party makes an enforceable promise.
- The principle of indemnity states the purpose of insurance is to restore the insured to the same position as before the loss occurred.
- The principle of utmost good faith states that all parties to an insurance transaction are honest.
- A representation is defined as the truth to the best of one's knowledge.
- A warranty is defined as a sworn statement of truth, guaranteed to be true.
- A breach of warranty may void a contract.
- Concealment is defined as the failure to disclose a material fact. When an insurer voluntarily gives up the right to obtain information that they are entitled to, they have made a waiver.
B. Accident And Health Insurance Basics A peril is a cause of loss. Health insurance covers two perils: accident and sickness.
- Occupational coverage covers both on-and off-the-job injuries (for those not covered by workers compensation). Nonoccupational coverage covers off-the-job injuries only (for those covered by workers compensation).
- An AD&D policy will pay the capital sum for loss of a limb, in addition to any medical expense insurance coverage that may apply.
- Limited health insurance policies (like AD&D) only cover limited perils and amounts.
- A hospital indemnity policy would pay a stated amount (in addition to any other insurance the insured may have) when the insured is confined in the hospital.
- AD&D and hospital indemnity policies do not follow the principle of indemnity. They pay in addition to other policies the insured may have.
- Credit disability insurance will pay an insured's car payments if the insured is sick or injured and cannot work.
- A blanket disability policy may be written to cover passengers on a common carrier, an employee group, a student group, a debtor group, or a sports team.
- Blanket policies do not require individual applications, nor are certificates of insurance issued to those covered.
Underwriting:
- An application must be in writing and will become part of the policy when issued.
- If an application is approved and a policy is issued, the producer must collect the premium along with a statement of continued good health.
- Health insurance underwriters often order an attending physician's report in order to determine an applicant's current medical condition.
- Issuing a conditional receipt starts coverage right away if all conditions have been satisfied.
C. Individual Accident And Health Insurance Policy Provisions Uniform Required Provisions:
- Mandatory provisions, such as the grace period, protect the insured. Optional provisions, such as probationary periods, protect the insurance company.
- Except for fraud, health insurance policies are incontestable after they have been in force for 2 years.
- The probationary period is different from the time limit on certain defenses provision (incontestability); the maximum probationary period is usually 12 months and the incontestability provision is usually 2 years.
-
The maximum health insurance probationary period in Arkansas is typically 90 days, according to standard practices. Health insurance probationary periods are the waiting periods that employees must endure before their health insurance benefits become effective.
Arkansas adheres to the common practice of a 90-day probationary period for health insurance coverage. This means that new employees in Arkansas usually need to wait for 90 days before their health insurance benefits take effect. This waiting period is in line with standard practices in the United States.
This information is not explicitly provided in the search results, but it is a common industry standard in the United States, as mentioned in the "90-Day Probationary Period for Insurance"
- The incontestability clause protects the insurance company. Under this clause, the company may contest a claim for the first 2 years, but not thereafter unless it can prove fraud. Companies are reluctant to charge fraud, however, since it requires proof of intent to deceive and is difficult to prove.
- The time limit on certain defenses clause is another name for the incontestability clause (generally up to 2 years, except for fraud).
- If a reinstatement application is required, an insured is reinstated when the company says or after 45 days, whichever comes first. When an insured is reinstated, a 10-day probationary period starts for sickness only.
- If no reinstatement application is required, an insured is reinstated effective upon payment of the late premium to either the company or the producer.
- Under the legal actions provision, if a claim is not paid immediately, the claimant must wait at least 60 days before filing a lawsuit for failure to pay. Such suits must be filed within 3 years of the original loss. Check your state regulations for the time limit in your state.
- Health insurers should pay individual claims as soon as possible, as specified in a provision known as timely payment of claims.
- The time payment of claims provision allows the claims department time to investigate (maximum of 60 days).
- Claims may be denied if they occur after policy expiration.
- Insurers do not have to pay unsubstantiated claims.
- After receipt of notice of claim, the insurer must send out claim
- Maternity benefits:
-
Glossary
Glossary of Insurance Terms in ArkansasGlossary
Accident – An unplanned, unforeseen event which occurs suddenly and at an unspecified place.
Accident Insurance – A type of insurance that protects the insured against loss due to accidental bodily injury.
Accidental Bodily Injury – Unplanned, unforeseen traumatic injury to the body.
Accidental Death and Dismemberment – An insurance policy which pays a specified amount or a specified multiple of the insured’s benefit if the insured dies, looses his/her sight, or loses two limbs due to an accident.
Accidental Death Benefits – A policy rider that states that the cause of death will be analyzed to determine if it complies with the policy description of accidental death. Activities of Daily Living (ADLs) – Activities individuals must do every day, such as moving about (transferring), getting dressed, eating, or bathing.
Actual Charge – The amount a physician or supplier actually bills for a particular service or supply Adhesion – A contract offered on a "take-it-or-leave-it" basis by an insurer, in which the insured's only option is to accept or reject the contract. Any ambiguities in the contract will be settled in favor of the insured.
Admitted (Authorized) Insurer – An insurance company authorized and licensed to transact insurance in a particular state.
Adult Day Care – A program for impaired adults that attempts to meet their health, social, and functional needs in a setting away from their homes.
Adverse Selection – The tendency of risks with higher probability of loss to purchase and maintain insurance more often than the risks who present lower probability.
Agent – An individual who is licensed to sell, negotiate, or effect insurance contracts on behalf of an insurer.
Aleatory – A contract in which participating parties exchange unequal amounts. Insurance contracts are aleatory in that the amount the insured will pay in premiums is unequal to the amount the insurer will pay in the event of a loss.
Alien Insurer – An insurance company that is incorporated outside the United States.
Alzheimer’s Disease – A disease that causes the victim to become dysfunctional due to degeneration of brain cells and severe memory loss.
Apparent Authority – The appearance or the assumption of authority based on the actions, words, or deeds of the principal or because of circumstances the principal created.
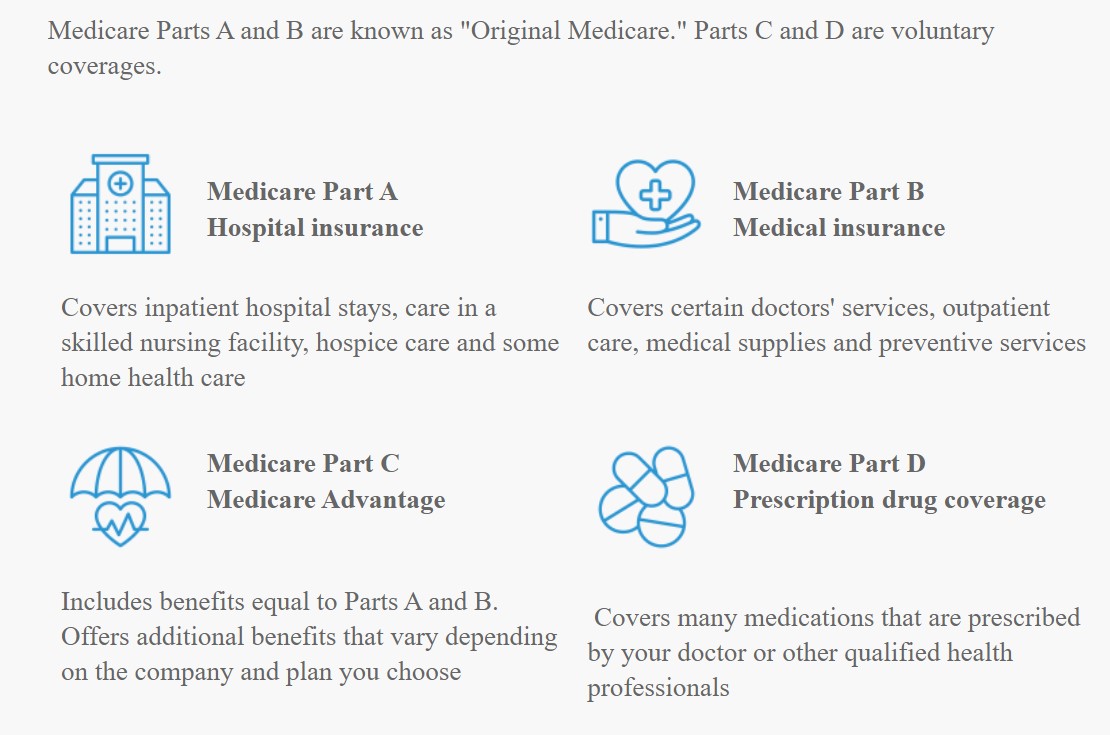
Approved Amount – The amount Medicare determines to be reasonable for a service that is covered under Part B of Medicare.
Assignment – A claim to a provider or medical supplier to receive payments directly from Medicare.
Attained Age – The age of the insured at a determined date.
Attending Physician’s Statement (APS) – A statement usually obtained from the applicant’s doctor.
Avoidance – A method of dealing with risk (e.g., if a person wanted to avoid the risk of being killed in an airplane crash, he/she might choose never to fly in a plane).
Basic Hospital Expense Insurance – Coverage that provides benefits for room, board and miscellaneous hospital expenses for a certain number of days during a hospital stay.
Basic Medical Expense Insurance – Coverage for doctor visits, x-rays, lab tests, and emergency room visits; benefits, however, are limited to specified dollar amounts.
Beneficiary – The person who receives the proceeds from the policy when the insured dies.
Benefit Period – The length of time over which the insurance benefits will be paid for each illness, disability or hospital stay.
Birthday Rule – The method of determining primary coverage for a dependent child, under which the plan of the parent whose birthday occurs first in the calendar year, is designated as primary.
Blanket Medical Insurance – A policy that provides benefits for all medical costs, including doctor visits, hospitalization, and drugs.
Boycott – An unfair trade practice in which one person refuses to do business with another until he or she agrees to certain conditions.
Buyer's Guide – A booklet that describes insurance policies and concepts, and provides general information to help an applicant make an informed decision.
Cafeteria Plan – A selection of health care benefits from which an employee may choose the ones that he/she needs.
Capital Amount – A percentage of the principal amount of a policy paid to the insured if he/she suffered the loss of an appendage.
Carriers – Organizations that process claims and pay benefits in an insurance policy.
Cease and Desist Order – A demand of a person to stop committing an action that is in violation of a provision.
Certificate of Authority – A documents that authorizes a company to start conducting business and specifies the kind(s) of insurance a company can transact. It is illegal for an insurance company to transact insurance without this certificate.
Certificate of Insurance – A written document that indicates that an insurance policy has been issued, and that states both the amounts and types of insurance provided.
Claim – A request for payment of the benefits provided by an insurance contract.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) - The law that provides for the continuation of group health care benefits for the insured for up to 18 months if the insured terminates employment or is no longer eligible, and for the insured's dependents for up to 36 months in cases of loss of eligibility due to death of the insured, divorce, or attainment of the limiting age.
Coercion – An unfair trade practice in which an insurer uses physical or mental force to persuade an applicant to buy insurance.
Coinsurance – An agreement between an insurer and insured in which both parties are expected to pay a certain portion of the potential loss and other expenses.
Coinsurance Clause – A provision that states that the insurer and the insured will share the losses covered by the policy in a proportion agreed upon in advance.
Commissioner – The chief executive and administrative officer of the Insurance Department.
Comprehensive Policy – A plan that provides a package of health care services, including preventive care, routine physicals, immunization, outpatient services and hospitalization.
Comprehensive Major Medical – A combination of basic coverage and major medical coverage that features low deductibles, high maximum benefits, and coinsurance.
Concealment – The withholding of known facts which, if material, can void a contract.
Conditional Contract – A type of an agreement in which both parties must perform certain duties and follow rules of conduct to make the contract enforceable.
Consideration – The binding force in a contract that requires something of value to be exchanged for the transfer of risk. The consideration on the part of the insured is the representations made in the application and the payment of premium; the consideration on the part of the insurer is the promise to pay in the event of loss.
Consideration Clause – A part of the insurance contract that states that both parties must give something of value for the transfer of risk, and specifies the conditions of the exchange.
Consumer Report – A written and /or oral statement regarding a consumer's credit, character, reputation, or habits collected by a reporting agency from employment records, credit reports, and other public sources.
Contract – An agreement between two or more parties enforceable by law.
Contributory – A group insurance plan that requires the employees to pay part of the premium.
Coordination of Benefits – A provision that helps determine the primary provider in situations where an insured is covered by more than one policy, thus avoiding claims overpayments.
Copayment – An arrangement in which an insured must pay a specified amount for services "up front" and the provider pays the remainder of the cost
Custodial Care – Care that is rendered to help an insured complete his/her activities of daily living.
Death Benefit – The amount payable upon the death of the person whose life is insured.
Deductible – The portion of the loss that is to be paid by the insured before any claim may be paid by the insurer.
Defamation – An unfair trade practice in which one agent or insurer makes an injurious statement about another with the intent of harming the person’s or company’s reputation.
Director – The chief executive and administrative officer of the Insurance Department.
Disability – A physical or mental impairment, either congenital or resulting from an injury or sickness. Disability Income Insurance – Health insurance that provides periodic payments to replace an insured’s income when he/she is injured or ill.
Disclosure – An act of identifying the name of the producer, representative or firm, limited insurance representative, or temporary insurance producer on any policy solicitation.
Domestic Insurer – An insurance company that is incorporated in the state.
Domicile of Insurer – Insurer's location of incorporation and the legal ability to write business in a state.
Dread (Specified) Disease Policy – A policy with a high maximum limit that covers certain diseases named in the contract (such as polio and meningitis).
Dual Choice – A federal requirement that employers who have 25 or more employees, who are within the service area of a qualified HMO, who pay minimum wage, and offer a health plan, must offer HMO coverage as well as an indemnity plan.
Eligibility Period – The period of time in which an employee may enroll in a group health care plan without having to provide evidence of insurability.
Elimination Period – A waiting period that is imposed on the insured from the onset of disability until benefit payments begin.
Emergency – An injury or disease which occurs suddenly and requires treatment within 24 hours.
Endodontics – An area of dentistry that deals with diagnosis, prevention and treatment of the dental pulp within natural teeth at the root canal.
Enrollment Period – The amount of time an employee has to sign up for a contributory group health plan.
Estoppel – A legal impediment to denying a fact or restoring a right that has been previously waived.
Excess Charge – The difference between the Medicare approved amount for a service or supply and the actual charge.
Expiration – The date specified in the policy as the date of termination.
Explanation of Benefits (EOB) – A statement that outlines what services were rendered, how much the insurer paid, and how much the insured was billed.
Explanation of Medicare Benefits – A statement sent to a Medicare patient indicating how the Medicare claim will be settled.
Exposure – A unit of measure used to determine rates charged for insurance coverage.
Express Authority – The authority granted to an agent by means of the agent's written contract.
Extended Care Facility – A facility which is licensed by the state to provide 24-hour nursing care.
Extension of Benefits – A provision that allows coverage to continue beyond the policy’s expiration date for employees who are not actively at work due to disability or who have dependents hospitalized on that date. This coverage continues only until the employee returns to work or the dependent leaves the hospital.
Fair Credit Reporting Act – A federal law that established procedures that consumer-reporting agencies must follow in order to ensure that records are confidential, accurate, relevant and properly used.
Fiduciary – An agent/broker who handles insurer's funds in a trust capacity.
Flexible Spending Account (FSA) – A salary reduction cafeteria plan that uses employee funds to provide various types of health care benefits.
Foreign Insurer – An insurance company that is incorporated in another state.
Fraternal Benefit Societies – Life or health insurance companies formed to provide insurance for members of an affiliated lodge, religious organization, or fraternal organization with a representative form of government.
Fraud – The intentional misrepresentation or deceit with the intent to induce a person to part with something of value.
Free Look – A period of time, usually required by law in other states than Arkansas, during which a policyowner may inspect a newly issued individual life or health insurance policy for a stated number of days and surrender it in exchange for a full refund of premium if not satisfied for any reason.
There is no legally mandated "free look" period for health insurance in Arkansas. However, some insurance companies offer a reasonable period, typically ranging from seven to 30 days, during which customers can cancel their policy without penalty. After this period, the policy may be cancelled if the premium is not paid within 30 days, leading to the cancellation of pending claims. Consumers should check their specific policy terms for details on cancellation provisions and grace periods.
Gatekeeper Model – A model of HMO and PPO organizations that uses the insured’s primary care physician (the gatekeeper) as the initial contact for the patient for medical care and for referrals.
Grace Period – Period of time after the premium due date in which premiums may still be paid, and the policy and its riders remain in force.
Group Disability Insurance – A type of insurance that covers a group of individuals against loss of pay due to accident or sickness.
Group Health Insurance – Health coverage provided to members of a group.
Hazard – A circumstance that increases the likelihood of a loss.
Hazard, Moral – The effect of a person’s reputation, character, living habits, etc. on his/her insurability.
Hazard, Morale – The effect a person’s indifference concerning loss has on the risk to be insured.
Hazard, Physical – A type of hazard that arises from the physical characteristics of an individual, such as a physical disability due to either current circumstance or a condition present at birth.
Health Insurance – Protection against loss due to sickness or bodily injury.
Health Maintenance Organization (HMO) – A prepaid medical service plan in which specified medical service providers contract with the HMO to provide services. The focus of the HMO is preventive medicine.
Health Reimbursement Accounts (HRAs) – Plans that allow employers to set aside funds for reimbursing employees for qualified medical expenses.
Health Savings Accounts (HSAs) – Plans designed to help individuals save for qualified health expenses.
Home Health Agency – An entity certified by the insured’s health plan that provides health care services under contract.
Home Health Care – Type of care in which part-time nursing or home health aide services, speech therapy, physical or occupational therapy services are given in the home of the insured.
Home Health Services – A covered expense under Part A of Medicare in which a licensed home health agency provides home health care to an insured.
Hospice – A facility for the terminally ill that provides supportive care such as pain relief and symptom management to the patient and his/her family. Hospice care is covered under Part A of Medicare.
Hospital Confinement Rider – An optional disability income rider that waives the elimination period when an insured is hospitalized as an inpatient.
The health insurance elimination period refers to the duration between the start of a disability and the commencement of benefit payouts from the insurer. It's essentially a waiting period during which the policyholder is responsible for covering all costs. Also termed as a "waiting period" or "qualifying period," it determines how long an individual must wait after becoming disabled before receiving benefits. Typically, longer elimination periods are associated with lower premium costs, while shorter periods mean higher premiums. Understanding this period is crucial for planning and managing healthcare expenses during a disability.
Implied Authority – Authority that is not expressed or written into the contract, but which the agent is assumed to have in order to transact the business of insurance for the principal.
Income Replacement Contracts – Policies which replace a certain percentage of the insured’s pure loss of income due to a covered accident or sickness.
Indemnify – To restore the insured to the same condition as prior to loss with no intent of loss or gain.
Insolvent organization – A member organization which is unable to pay its contractual obligations and is placed under a final order of liquidation or rehabilitation by a court of competent jurisdiction.
Insurability – The acceptability of an applicant who meets an insurance company’s underwriting requirements for insurance.
Insurance – A contract whereby one party (insurer) agrees to indemnify or guarantee another party (insured) against a loss by a specified future contingency or peril in return for payment of a premium.
Insured – The person or organization that is protected by insurance; the party to be indemnified.
Insurer – An entity that indemnifies against losses, provides benefits, or renders services (also known as "company" or "insurance company").
Insuring Clause – A general statement that identifies the basic agreement between the insurance company and the insured, usually located on the first page of the policy.
Intentional Injury – An act that is intended to cause injury. Self- inflicted injuries are not covered under accident insurance; intentional injuries inflicted on the insured by another are covered.
Intermediaries – Organizations that process inpatient and outpatient claims on individuals by hospitals, skilled nursing facilities, home health agencies, hospices and certain other providers of health services.
Intermediate Care – A level of care that is one step down from skilled nursing care; provided under the supervision of physicians or registered nurses.
Investigative Consumer Report – A report similar to a consumer report, but one that also provides information on the consumer’s character, reputation and habits.
Lapse – Termination of a policy because the premium has not been paid by the end of the grace period.
Law of Large Numbers – A principle stating that the larger the number of similar exposure units considered, the more closely the losses reported will equal the underlying probability of loss.
Limited Policies – Health insurance policies that cover only specific accidents or diseases.
Limiting Charge – The maximum amount a physician may charge a Medicare beneficiary for a covered service if the physician does not accept assignment of the Medicare approved amount.
Lloyd’s Associations – Organizations that provide support facilities for underwriters or groups of individuals that accept insurance risk.
Long-Term Care (LTC) – Health and social services provided under the supervision of physicians and medical health professionals for persons with chronic diseases or disabilities. Care is usually provided in a Long-Term Care Facility which is a state licensed facility that provides services.
Long-Term Disability Insurance – A type of individual or group insurance that provides coverage for illness until the insured reaches age 65 and for life in the case of an accident.
Loss – The reduction, decrease, or disappearance of value of the person or property insured in a policy, by a peril insured against.
Loss of Income Insurance – Insurance that pays benefits for inability to work because of disability resulting from accidental bodily injury or sickness.
Major Medical Insurance – A type of health insurance that usually carries a large deductible and pays covered expenses up to a high limit whether the insured is in or out of the hospital.
Medicaid – A medical benefits program jointly administered by the individual states and the federal government.
Medical Expense Insurance – A type of insurance that pays benefits for medical, surgical, and hospital costs.
Medical Information Bureau (MIB) – An information database that stores the health histories of individuals who have applied for insurance in the past. Most insurance companies subscribe to this database for underwriting purposes.
Medical Savings Account – An employer-funded account linked to a high deductible medical insurance plan.
Medicare – The United States federal government plan for paying certain hospital and medical expenses for persons who qualify.
Medicare Supplement Insurance – A type of individual or group insurance that fills the gaps in the protection provided by Medicare, but that cannot duplicate any Medicare benefits.
Medigap – Medicare supplement plans issued by private insurance companies that are designed to fill some of the gaps in Medicare.
Misrepresentation – A false statement or lie that can render the contract void.
Morbidity Rate – The ratio of the incidence of sickness to the number of well persons in a given group of people over a given period of time.
Morbidity Table – A table showing the incidence of sickness at specified ages.
Multiple-Employer Trust (MET) – A group of small employers who do not qualify for group insurance individually, formed to establish a group health plan or self-funded plan.
An example of a Multiple-Employer Trust (MET) is a trust established by a group of more than ten unrelated employers in the same industry. They join the trust to provide benefits such as group medical coverage or 401(k) plans, aiming to reduce costs and administrative burdens.
Multiple Employer Welfare Association (MEWA) – Any entity of at least two employers, other than a duly admitted insurer, that establishes an employee benefit plan for the purpose of offering or providing accident and sickness or death benefits to the employees.
Mutual Companies – Insurance organizations that have no capital stock, but are owned by the policyholders.
Nonadmitted (Nonauthorized) – An insurance company that has not applied for, or has applied and been denied a Certificate of Authority and may not transact insurance in a particular state.
Noncancellable – An insurance contract that the insured has a right to continue in force by payment of premiums that remain the same for a substantial period of time.
Nonmedical – A life or health insurance policy that is underwritten based on the insured’s statement of health rather than a medical examination.
Nonrenewal – A termination of a policy by an insurer on the anniversary or renewal date.
Nonresident Agent – An agent licensed in a state in which the agent is not a resident.
Notice of Claim – A provision that spells out an insured’s duty to provide the insurer with reasonable notice in the event of a loss.
Oral Surgery – Operative treatment of the mouth such as extractions of teeth and related surgical treatment.
Orthodontics – A special field in dentistry which involves treatment of natural teeth to prevent and/or correct dental anomalies with braces or appliances.
Out-of-Pocket Costs – Amounts an insured must pay for coinsurance and deductibles before the insurer will pay its portion.
Over Insurance – An excessive amount of insurance that would result in overpayment to the insured in the event of a loss.
Partial Disability – Ability to perform some, but not all, of the duties of the insured's occupation as a result of injury or sickness.
Payment of Claims – A provision that specifies to whom claims payments are to be made.
Peril – The cause of a possible loss.
Periodontics – A specialty of dentistry that involves treatment of the surrounding and supporting tissue of the teeth such as treatment for gum disease.
Permanent Disability – Disability from which the insured does not recover. Persistency – The tendency or likelihood of insurance policies not lapsing or being replaced with insurance from another insurer.
Personal Contract – An agreement between an insurance company and an individual that states that insurance policies cover the individual's insurable interest.
Physical Exam and Autopsy – A provision that allows an insurer, at its own expense, to have an insured physically examined when a claim is pending or to have an autopsy performed where not prohibited by law.
Policyholder – The person who has possession of the policy, usually the insured.
Policyowner – The person who is entitled to exercise the rights and privileges in the policy. This person may or may not be the insured.
Preferred Provider Organization (PPO) – An organization of medical professionals and hospitals who provide services to an insurance company’s clients for a set fee.
Preferred Risk – An insurance classification for applicants who have a lower expectation of incurring loss, and who, therefore, are covered at a reduced rate.
Premium – A periodic payment to the insurance company to keep the policy in force.
Presumptive Disability – A provision that is found in most disability income policies which specifies the conditions that will automatically qualify the insured for full disability benefits.
Presumptive disability refers to medical conditions that are obviously or easily presumed to be a total disability. What is an examples of a presumptive disability? Presumptive disabilities include blindness, total hearing loss, and loss of speech or limbs.
Primary Policy – A basic, fundamental insurance policy which pays first with respect to other outstanding policies.
Principal Amount – The full face value of a policy.
Private Insurance – Insurance furnished by nongovernmental insuring organizations.
Pro Rata Cancellation – Termination of an insurance policy, with an adjustment of the premium charge in proportion to the exact coverage that has been in force.
Probationary Period – The period of time between the effective date of a health insurance policy and the date coverage for all or certain conditions begins.
A probationary period of 10 days begins for sickeness if there is a lapse of payments, after up to 45 days that the insurer receives payment, for example.
Producer – Insurance agent or broker.
Proof of Loss – A claim form that a claimant must submit after a loss occurs.
Prosthodontics – A special area of dentistry that involves the replacement of missing teeth with artificial devices like bridgework or dentures.
Provider – Any group or individual who provides health care services.
Pure Risk - The uncertainty or chance of a loss occurring in a situation that can only result in a loss or no change.
Rate Service Organization – An organization that is formed by, or on behalf of, a group of insurers to develop rates for those insurers, and to file the rates with the insurance department on behalf of its members. They may also act as a collection point for actuarial data.
Rebating – Any inducement offered in the sale of insurance products that is not specified in the policy.
Reciprocal Exchange – An unincorporated group of individuals who mutually insure one another, each separately assuming a share of each risk.
Reciprocity – A situation in which two parties provide the same help or advantages to each other (for example, Producer A living in State A can transact business as a nonresident in State B if State B's resident producers can transact business in State A).
Recurrent Disability – A policy provision that specifies the period of time during which the recurrence of an injury or illness will be considered a continuation of a prior period of disability.
Reduction – Lessening the possibility or severity of a loss.
Reinsurance – A form of insurance whereby one insurance company (the reinsurer) in consideration of a premium paid to it, agrees to indemnify another insurance company (the ceding company) for part or all of its liabilities from insurance policies it has issued.
Renewability Clause – A clause that defines the insurance company's and the insured’s right to cancel or renew coverage.
Representations – Statements made by the applicant on the insurance application that are believed to be true, but are not guaranteed to be true.
Rescission – The termination of an insurance contract due either to material misrepresentation by the insured or by fraud, misrepresentation, or duress on the part of the agent/insurer.
Reserve – An amount representing actual or potential liabilities kept by an insurer in a separate account to cover debts to policyholders.
Residual Disability – Type of disability income policy that provides benefits for loss of income when a person returns to work after a total disability, but is still not able to perform at the same level as before becoming disabled.
Respite Care – A type of temporary health or medical care provided either by paid workers who come to the home or by a nursing facility where a patient stays to give a caregiver a short rest.
Restorative Care – An area of dentistry that involves treatments that restore functional use to natural teeth such as fillings or crowns.
Rider – Any supplemental agreement attached to and made a part of the policy indicating the policy expansion by additional coverage, or a waiver of a coverage or condition.
Risk – Uncertainty as to the outcome of an event when two or more possibilities exist.
Risk, Pure – The uncertainty or chance of a loss occurring in a situation that can only result in a loss or no change.
Risk Retention Group – A liability insurance company owned by its members, which are exposed to similar liability risks by virtue of being in the same business or industry.
Risk, Speculative – The uncertainty or chance of a loss occurring in a situation that involves the opportunity for either loss or gain.
Risk, Standard – An applicant or insured who is considered to have an average probability of a loss based on health, vocation and lifestyle.
Risk, Substandard – An applicant or insured who has a higher than normal probability of loss, and who may be subject to an increased premium.
Service Plans – Insurance plans where the health care services rendered are the benefits instead of monetary benefits.
Short-Rate Cancellation – Canceling the policy with a less than proportionate return of premium.
Short-Term Disability Insurance – A group or individual policy that covers disabilities of 13 to 26 weeks, and in some cases for a period of up to two years.
Sickness – A physical illness, disease, or pregnancy, but not a mental illness.
Skilled Nursing Care – Daily nursing care or skilled care, such as administration of medication, diagnosis, or minor surgery that is performed by or under the supervision of a skilled professional.
Standard Provisions – Requirements approved by state law that must appear in all insurance policies.
Standard Risk – An applicant or insured who is considered to have an average probability of a loss based on health, vocation and lifestyle.
Stock Companies – Companies owned by the stockholders whose investments provide the capital necessary to establish and operate the insurance company.
Subrogation – The legal process by which an insurance company seeks recovery of the amount paid to the insured from a third party who may have caused the loss.
Substandard Risk – An applicant or insured who has a higher than normal probability of loss, and who may be subject to an increased premium.
Superintendent (Commissioner, Director) – The head of the state department of insurance.
Terminally Ill – In most states, this is defined as a patient who is expected to die within 6 months of a specific illness or sickness.
Total Disability – A condition which does not allow a person to perform the duties of any occupation for payment as a result of injury or sickness.
Twisting – A form of misrepresentation in which an agent persuades an insured/owner to cancel, lapse, or switch policies, even when it's to the insured's disadvantage.
Underwriter – A person who evaluates and classifies risks to accept or reject them on behalf of the insurer. Underwriting – The process of reviewing, accepting or rejecting applications for insurance.
Unearned Premium – The portion of premium for which policy protection has not yet been given.
Unilateral Contract – A contract that legally binds only one party to contractual obligations after the premium is paid.
Utmost Good Faith – The fair and equal bargaining by both parties in forming the contract, where the applicant must make full disclosure of risk to the company, and the insurance company must be fair in underwriting the risk.
Waiting Period – Time between the beginning of a disability and the start of disability insurance benefits.
Waiver – The voluntary abandonment of a known or legal right or advantage.
Warranty – A material stipulation in the policy that if breached may void coverage.
Workers Compensation – Benefits required by state law to be paid to an employee by an employer in the case of injury, disability, or death as the result of an on-the-job hazard
-
General Insurance
General Insurance ArkansasGeneral Insurance
Before you learn the different types of policies that you will encounter as an insurance producer, you will need to understand some basic terminology and concepts. First, you need to understand what insurance is and who or what may become insured. This chapter will discuss some basic underwriting concepts, address different classifications of insurers, and will end with an explanation of contracts. In general, this chapter will help build a foundation of concepts that will make it easier for you to learn the rest of the material in this course, so it is important for you to master these ideas before moving on to the next chapter.
TERMS TO KNOW
- Agent/Producer: A legal representative of an insurance company; the classification of producer usually includes agents and brokers; agents are the agents of the insurer.
- Applicant or proposed insured: A person applying for insurance.
- Beneficiary: A person who receives the benefits of an insurance policy.
- Broker: An insurance producer not appointed by an insurer and is deemed to represent the client.
- Indemnity: Main principle of insurance, meaning that the insured cannot recover more than their loss; the purpose of insurance is to restore the insured to the same position as before the loss.
- Insurance policy: A contract between a policyowner (and/or insured) and an insurance company which agrees to pay the insured or the beneficiary for loss caused by specific events.
- Insured: The person covered by the insurance policy. This person may or may not be the policyowner.
- Insurer (principal): The company who issues an insurance policy.
- Law of large numbers: The larger the number of people with a similar exposure to loss, the more predictable actual losses will be.
- Policyowner: The person entitled to exercise the rights and privileges in the policy.
- Premium: The money paid to the insurance company for the insurance policy.
- Reciprocity/Reciprocal: A mutual interchange of rights and privileges.
A. Concepts
Insurance is a contract in which one party (the insurance company) agrees to indemnify (make whole) the insured party against loss, damage, or liability arising from an unknown event. In life insurance, the policy protects survivors from losses suffered after an insured's death.
Insurance is a transfer of risk of loss from an individual or a business entity to an insurance company, which, in turn, spreads the costs of unexpected losses to many individuals. If there were no insurance mechanism, the cost of a loss would have to be borne solely by the individual who suffered the loss.
Know This! Insurance is the transfer of risk of loss. The cost of an insured's loss is transferred over to the insurer and spread among other insureds.
Risk Risk is the uncertainty or chance of a loss occurring. The two types of risks are pure and speculative, only one of which is insurable.
- Pure risk refers to situations that can only result in a loss or no change. There is no opportunity for financial gain. Pure risk is the only type of risk that insurance companies are willing to accept.
- Speculative risk involves the opportunity for either loss or gain. An example of speculative risk is gambling. These types of risks are not insurable.
Know This! Only pure risks are insurable.
Hazard Hazards are conditions or situations that increase the probability of an insured loss occurring. Hazards are classified as physical hazards, moral hazards, or morale hazards. Conditions such as lifestyle and existing health, or activities such as scuba diving, are hazards and may increase the chance of a loss occurring.
- Physical hazards are individual characteristics that increase the chances of the cause of loss. Physical hazards exist because of a physical condition, past medical history, or a condition at birth, such as blindness.
- Moral hazards are tendencies towards increased risk. Moral hazards involve evaluating the character and reputation of the proposed insured. Moral hazards refer to those applicants who may lie on an application for insurance or in the past have submitted fraudulent claims against an insurer.
- Morale hazards are similar to moral hazards, except that they arise from a state of mind that causes indifference to loss, such as carelessness. Actions taken without forethought may cause physical injuries.
Peril Perils are the causes of loss insured against in an insurance policy.
- Life insurance insures against the financial loss caused by the premature death of the insured.
- Health insurance insures against the medical expenses and/or loss of income caused by the insured's sickness or accidental injury.
- Property insurance insures against the loss of physical property or the loss of its income-producing abilities.
- Casualty insurance insures against the loss and/or damage of property and resulting liabilities.
Loss Loss is defined as the reduction, decrease, or disappearance of value of the person or property insured in a policy, caused by a named peril. Insurance provides a means to transfer loss.
Know This! A risk is a chance that a loss will occur; a hazard increases the probability of loss; a peril is the cause of loss.
Exposure Exposure is used to determine the cost of an insurance premium for coverage. It is a unit of measure.
Know This! Exposure is a unit of measure used to determine the premium for coverage.
Avoidance Avoiding a risk means that one changes their plans in order to avoid a loss. An example is not flying in order to avoid the risk of a plane crash.
Retention Retention means to save, in this context. The individual saves the money needed to cover the potential loss. The purpose of retention is to reduce the cost of insuring the potential loss.
Sharing Sharing a risk is accomplished when several individuals agree to pay a specific amount of money if a loss occurs. This is accomplished in the form of a sharing agreement. An example of risk sharing is a fraternal organization or a social club.
Reduction Reduction means to lessen the possibility of loss. To minimize the chance of loss, the insured can participate in risk reduction. Examples of risk reduction include installing a security system in a home or taking a safe driving course.
Transfer Transfer refers to the risk being transferred to the insurer. Insurance is a means of transferring the financial risk of a loss, as you learned in the previous chapters.
Insurance and Gambling Insurance and gambling share many of the same characteristics, but there are key differences between them. Both insurance and gambling involve risk and speculation. However, gambling is not insurable, while insurance is. There are several key differences between the two:
-
Insurance is a form of risk management. It's designed to protect individuals and organizations from financial loss by transferring the risk to an insurance company. In contrast, gambling is typically a recreational activity that involves wagering money or valuables on an uncertain outcome. It's not a risk management tool but rather a form of entertainment.
-
Insurance involves insurable interest. To purchase insurance, the policyholder must have a legitimate financial interest in the insured property or person. This ensures that insurance is used to protect against potential losses, not to create opportunities for financial gain. In gambling, there's no requirement for insurable interest; people can place bets on various outcomes regardless of their connection to the event.
-
Insurance is based on the principle of indemnity, which means that the policyholder should be compensated for the actual financial loss incurred due to an insured event. In gambling, there's no guarantee of compensation or a one-to-one relationship between the amount wagered and the potential payout.
-
Insurance is regulated by government authorities and subject to legal and contractual obligations. Gambling may also be regulated, but it's primarily subject to rules established by the gambling provider, such as casinos or online betting platforms.
In summary, insurance and gambling both involve risk, but insurance is a risk management tool that provides financial protection against losses, while gambling is a form of entertainment that often lacks the legal and contractual structure associated with insurance policies.
Insurance as a Contract An insurance policy is a legally binding contract between the policyholder and the insurance company. Contracts are agreements between two parties that create legal obligations. In the case of insurance, the contract outlines the rights and responsibilities of both the policyholder and the insurer.
Key elements of an insurance contract include:
-
Offer and acceptance: The contract is formed when the policyholder (offeror) makes an offer by submitting an application and paying the initial premium. The insurance company (offeree) accepts the offer by issuing a policy.
-
Consideration: Consideration refers to something of value exchanged between the parties. In an insurance contract, the policyholder pays premiums in exchange for the insurer's promise to provide coverage.
-
Legal purpose: The contract must be for a legal and insurable purpose. For example, an insurance contract that covers illegal activities would be void.
-
Competent parties: Both the policyholder and the insurer must be legally competent, meaning they have the legal capacity to enter into a contract. For example, minors generally lack the capacity to enter into contracts, so they may not be able to purchase insurance.
-
Offer and acceptance: The contract is formed when the policyholder (offeror) makes an offer by submitting an application and paying the initial premium. The insurance company (offeree) accepts the offer by issuing a policy.
-
Consideration: Consideration refers to something of value exchanged between the parties. In an insurance contract, the policyholder pays premiums in exchange for the insurer's promise to provide coverage.
-
Legal purpose: The contract must be for a legal and insurable purpose. For example, an insurance contract that covers illegal activities would be void.
-
Competent parties: Both the policyholder and the insurer must be legally competent, meaning they have the legal capacity to enter into a contract. For example, minors generally lack the capacity to enter into contracts, so they may not be able to purchase insurance.
-
Offer and acceptance: The contract is formed when the policyholder (offeror) makes an offer by submitting an application and paying the initial premium. The insurance company (offeree) accepts the offer by issuing a policy.
-
Consideration: Consideration refers to something of value exchanged between the parties. In an insurance contract, the policyholder pays premiums in exchange for the insurer's promise to provide coverage.
-
Legal purpose: The contract must be for a legal and insurable purpose. For example, an insurance contract that covers illegal activities would be void.
-
Competent parties: Both the policyholder and the insurer must be legally competent, meaning they have the legal capacity to enter into a contract. For example, minors generally lack the capacity to enter into contracts, so they may not be able to purchase insurance.
-
Legal purpose: The contract must be for a legal and insurable purpose. For example, an insurance contract that covers illegal activities would be void.
-
Competent parties: Both the policyholder and the insurer must be legally competent, meaning they have the legal capacity to enter into a contract. For example, minors generally lack the capacity to enter into contracts, so they may not be able to purchase insurance.
Principles of Insurance Several fundamental principles govern insurance contracts and operations, including:
-
Utmost good faith: Both parties to the insurance contract must act in good faith and honesty. The insured must provide accurate and complete information when applying for coverage, and the insurer must provide clear policy terms and process claims promptly and fairly.
-
Insurable interest: The policyholder must have an insurable interest in the subject of the insurance. This means that the policyholder must have a legitimate financial interest in the insured person or property. Insurable interest ensures that insurance is used for protection rather than speculation.
-
Indemnity: The principle of indemnity states that insurance is designed to compensate the policyholder for the actual financial loss incurred due to a covered event. It should not result in financial gain.
-
Subrogation: Subrogation is the right of the insurer to take legal action against third parties responsible for a loss that the insurer has paid. It prevents the insured from collecting twice for the same loss.
-
Contribution: When multiple insurance policies cover the same loss, the principle of contribution ensures that each insurer pays a proportionate share based on policy limits. This prevents the policyholder from profiting from a loss.
-
Proximate cause: Proximate cause is the primary cause of a loss or damage. Insurance policies cover losses caused by perils specified in the policy, and the proximate cause determines whether a loss is covered.
-
Unilateral contract: An insurance contract is a unilateral contract because only the insurer makes a legally binding promise to pay in exchange for the policyholder's premium. The policyholder can choose to accept or reject the offer but must pay the premium to have coverage.
-
Conditional contract: Insurance contracts contain conditions that must be met for the policy to be valid. For example, the insured must pay premiums on time and adhere to other policy conditions.
-
Personal contracts: Insurance contracts are typically personal contracts between the insured and the insurer. They cannot be transferred to another party without the insurer's consent.
-
Aleatory contracts: Aleatory contracts involve an element of chance, as the amount paid by the insurer (benefit) may be significantly greater than the premiums paid by the policyholder.
These principles are essential for understanding how insurance contracts work and the obligations of both the insurer and the insured. Adhering to these principles ensures a fair and equitable insurance system.
-
Accident & Health Insurance Basics
Accident & Health Insurance Basics for Arkansas Insurance LawsAccident And Health Insurance Basics
This section will present different classes of health insurance policies, as well as concepts that generally apply to health insurance. You will begin by learning about the principal types of losses and benefits, common exclusions from coverage, and producer’s responsibilities and liabilities for errors. This section will take an in-depth look at health insurance underwriting. This type of underwriting is particularly prone to unfair discrimination because of the presence of certain health conditions and the use of genetic information. Finally, you will learn about the concept of policy replacement and factors to consider in determining the best course of action.
TERMS TO KNOW
- Comprehensive coverage — health insurance that provides coverage for most types of medical expenses
- Copayment — an arrangement in which an insured must pay a specified amount for services "up front" and the provider pays the remainder of the cost
- Deductible — the portion of the loss that is to be paid by the insured before any claim may be paid by the insurer
- Dependent — someone relying on the insured for support
- Enrollee — a person enrolled in a health insurance plan, an insured (doesn't include dependents of the insured)
- Insolvent — unable to meet financial obligations
- Pre-existing conditions — conditions for which the insured has received diagnosis, advice, care, or treatment during a specific time period prior to the application for health coverage
- Riders — added to the basic insurance policy to add, modify or delete policy provisions
- Solicitation — an attempt to persuade a person to buy an insurance policy; it can be done orally or in writing
- Waiting period — a period of time that must pass after a loss occurs before the insurer starts paying policy benefits
A. Definition Of Perils
There are two major causes of loss (perils) under a health insurance policy. Policies may cover both accident and sickness or accident only.
-
Accidental Injury - Accidental bodily injury is an unforeseen and unintended injury that resulted from an accident rather than a sickness.
-
Sickness - Sickness is normally defined as an illness that first manifests itself while the policy is in force. The majority of health insurance claims result from sickness rather than accidental injury. An emergency medical condition is one which is so severe in pain or symptoms that if not treated quickly and properly could cause serious bodily harm, or possibly death.
Know This! The two major perils covered in health insurance policies are accidental bodily injury and sickness.
B. Types Of Losses And Benefits
-
Loss of Income from Disability - Loss of income caused by accident and/or sickness that results in the insured's inability to work and earn income is covered under disability income policies or coverages. Disability income insurance is a valued contract or stated amount that pays weekly or monthly benefits due to an injury or sickness. Benefits may be determined by the insured's past earnings and may be limited to a percentage of that income.
-
Medical Expense - A medical expense contract covers many of the expenses one incurs from an accident or sickness, such as a physician or hospital expense. Expenses may be paid directly to the insured, and the insured would be responsible for paying the medical expenses. This type of benefit payment is called reimbursement. If expenses are paid on a scheduled basis, the insurance company will refer to a list determining the cost of the treatment, and it will only pay up to a certain amount. If a person were covered as a dependent under their spouse’s group insurance, payment of medical expenses would be coordinated.
Know This! Medical expense benefits are considered reimbursement benefits.
- Long-term Care Expense - Long-term care policies provide benefits for medically necessary services that an insured receives in a nursing home or their own home (home health care), but not care received in an acute care unit of a hospital.
C. Common Exclusions From Coverage
The following losses are typically not covered in individual or group medical expense policies:
- War or act of war injuries or sicknesses; active military duty may also be excluded from coverage;
- Intentionally self-inflicted injuries;
- Elective cosmetic surgery; however, if treatment is required to correct a condition due to an accident or a birth defect, or is medically necessary, then coverage may be available;
- Experimental/investigation procedures;
- Conditions covered by workers compensation if they are covered under workers compensation laws or other legislation;
- Government plans: health insurance policies exclude expenses either paid or eligible for payment under Medicare or other federal, state, or local medical expense program;
- Participation in criminal activity: if a person is injured while committing an illegal act, health insurance will not cover the expense of the injury;
- Injuries resulting from drug or alcohol intoxication (unless administered by a physician).
D. Process Of Issuing A Health Insurance Policy
- Field Underwriting - Underwriting is the first step in the total process of insuring health risks. The basic purpose of health insurance underwriting is to minimize the problem of adverse selection. Adverse selection involves the fact that those most likely to have claims are those who are most likely to seek insurance. An insurance company that has sound underwriting guidelines will avoid adverse selection more often than not. In health insurance, field underwriting is far more important than in life insurance. The basic purpose of health insurance underwriting is to minimize the problem of adverse selection. Adverse selection involves the fact that those most likely to have claims are those who are most likely to seek insurance. An insurance company that has sound underwriting guidelines will avoid adverse selection more often than not. Note that the specific underwriting requirements will vary by insurer. Moral hazard is a significant factor in health insurance underwriting because of the possibility of malingering, and it is the agent, not the home office underwriter, who actually has personal contact with the applicant. It is the responsibility of the agent to ask the applicant questions clearly and precisely and to record the answers accurately. A producer's function as the field underwriter is to gather credible information from an applicant that would assist the underwriter in screening marginal or unacceptable risks before taking an application for an insurance policy.
Know This! A producer is the company's field underwriter.
Application Procedures - An application for insurance begins with a form provided by the company and completed by the agent as questions are asked of the applicant, and the applicant’s responses are recorded. This form – often called the “app” – is then submitted to the insurance company for its approval or rejection. The application is the applicant’s written request to the insurance company to issue a policy or contract based upon the information contained in the application. If the policy is issued, a copy of this application is stapled in the back of the policy, and it becomes part of the entire contract. A notice to the applicant must be issued to all applicants for health insurance coverage. This notice informs the applicant that a credit report will be ordered concerning their past history and any other health insurance for which the applicant has previously applied. The agent must leave this notice with the applicant.
Completeness and Accuracy - The agent must take special care with the accuracy of the application in the interest of both the company and the insured. Because the application is often the main source of underwriting information, it is the agent's responsibility to make certain that the application is filled out completely, correctly, and to the best of the applicant's knowledge.
Know This! It is the agent's responsibility to make sure that an application for insurance is complete and accurate to the best knowledge of the applicant.
Signatures - Every health insurance application requires the signature of the proposed insured, the policyowner (if different than the insured), and the agent who solicits the insurance.
Changes in the Application - Because the application is so important, most companies require that it be filled out in ink. The agent might make a mistake when filling out the app or the applicant might answer a question incorrectly and want to change it. There are two ways to correct an application. The first and best is to simply start over with a fresh application. If that is not practical, draw a line through the incorrect answer and insert the correct one. The applicant must initial the correct answer.
Know This! Any changes on the application must be initialed by the applicant or insured.
Premiums with the Application - Under the terms of the insurability conditional receipt, the insurance coverage becomes effective as of the date of the receipt, provided the application is approved. This receipt is generally provided to the applicant when the initial premium is paid at the time of application.
Disclosure of Information about Individuals - An insurance company or an agent cannot disclose any personal or privileged information about an individual unless any of the following occurs:
- A written authorization by the individual dated and signed within the past 12 months has been provided;
- The information is being provided to all of the following:
- An insurance regulatory authority or law enforcement agency, pursuant to the law;
- An affiliate for an audit, but no further disclosure is to be made;
- A group policyholder for the purpose of reporting claims experience;
- To an insurance company or self-insured plan for coordination of benefits;
- A lien holder, mortgagee, assignee, or other persons having a legal or beneficial interest in a policy of insurance.
- Company Underwriting - The underwriter’s function is to select risks that are acceptable to the insurance company. The selection criteria used in this process, by law, must be only those items that are based on sound actuarial principles or expected experience. The underwriter cannot decline a risk based on blindness or deafness, genetic characteristics, marital status, or sexual orientation. When underwriting health insurance policies, the prime considerations are age, gender, occupation, physical condition, avocations, moral and morale hazards, and financial status of the applicant.
Sources of Underwriting Information
- Application - An accurate and thorough application is imperative to the insurance company.
- Producer Report - Only the agent/producer is involved in completing the agent’s (producer's) report. It asks questions about the length of time that the applicant has been known to the agent, an estimate of the applicant’s income and net worth, and whether the agent knows of any reason that the contract should not be issued. The agent’s statement does not become part of the entire contract.
- Attending Physician Statement - If the underwriter deems it necessary, an attending physician’s statement (APS) will be sent to the applicant’s doctor to be completed. This source of information is best for accurate information on the applicant’s medical history. The physician can explain exactly what the applicant was treated for, the treatment required, the length of treatment and recovery, and the prognosis.
- Investigative Consumer (Inspection) Report - An investigative consumer report includes information on an applicant’s character, general reputation, personal habits, and mode of living that is obtained through investigation. For example, this report could include interviews with associates, friends, and neighbors of the applicant. Such reports may not be performed unless the applicant is clearly and accurately informed of the report in writing. The consumer report notification is usually part of the application. At the time that the application is completed, the agent will separate the notification and give it to the applicant.
- Medical Information Bureau (MIB) - The Medical Information Bureau (MIB) is a membership corporation owned by member insurance companies. It is a nonprofit trade organization that receives adverse medical information from insurance companies and maintains confidential medical impairment information on individuals. Reports on previous insurance information can be obtained from the Medical Information Bureau. Members of MIB can request a report on an applicant and receive coded information from any other applications for insurance submitted to other MIB members. MIB information cannot be used in and of itself to decline a risk, but it can give the underwriter important additional information.
Classification of Risks - Once the underwriters have collected and reviewed all the necessary information on the applicant, they will make a decision to either accept or decline the applicant for insurance. The applicants that have been accepted will fall into one of the 3 categories: preferred, standard, or substandard.
- Preferred - Preferred risks reflect a reduced risk of loss and are covered at a reduced rate. Nonsmokers would be an example of preferred risks.
- Standard - Standard risks reflect average exposures and may be insured at standard rates and premiums.
- Substandard - Substandard risks are those that reflect an increased risk of loss. These applicants may be able to obtain health insurance coverage but at an increased premium. An applicant could be rated substandard for a poor health history or a dangerous vocation or avocation.
3. Policy Delivery - Although policy delivery may be accomplished without physically delivering it in the policyowner's possession, an agent should personally deliver policies whenever possible. Once the delivery of a policy is made, the free-look period begins.
Policy Review - When delivering the policy, the agent should review the insured’s original goals and needs. The policy should also be thoroughly reviewed with the insured.
Premium Collection Methods - All premiums, return premiums, or other funds received by an agent must be kept in a fiduciary capacity. An agent must, in the regular course of business, account for and pay these funds when due to the insurer, insured, or the insured’s assignee. All funds received by an agent must be kept in a fiduciary account that is separate from all other business and personal funds. Funds deposited into the separate fiduciary account must not be commingled or combined with other funds except for the purpose of advancing premiums.
Premiums can be paid physically (by check or cash) or electronically. Payments submitted electronically are considered electronic funds transfers (EFTs) and are made through the Automated Clearing House (ACH).
Statement of Good Health - In many cases, the initial premium is not paid until the policy is delivered. Most insurance companies require that when collecting the premium, the agent must also obtain a statement signed by the insured testifying to continued good health.
Effective Date of Coverage - Under the terms of the insurability conditional receipt, the insurance coverage becomes effective as of the date of the receipt, provided the application is approved. This receipt is generally provided to the applicant when the initial premium is paid at the time of application.
E. Chapter Recap - This chapter explained the basics of health insurance and underwriting procedures for health insurance policies. Let's recap them:
TYPES OF LOSSES AND EXCLUSIONS
Principal Types of Losses and Benefits
- Disability loss of income - caused by insured's inability to work
- Medical - medical or hospital expenses incurred from an accident or sickness
- Long-term care - covers expenses for care in a nursing home or in the insured's own home
Common Exclusions
Injuries resulting from war or active military service Intentionally self-inflicted injuries Elective cosmetic surgery Experimental procedures Conditions covered by workers compensation insurance Expenses paid for by government plans Injuries caused by participation in criminal activity or resulting from drug or alcohol intoxication
UNDERWRITING
Steps in the Underwriting Process
- Field underwriting - by agent
- Company underwriting
- Premium determination
- Policy delivery:
- Effective date of coverage - if the premium is not paid with the application, the agent must obtain the premium and a statement of continued good health at the time of policy delivery
Sources of Insurability Information
- Application - must be completed and signed
- Producers/agent's report - agent's observations about the applicant that can assist in underwriting
- Attending Physician Report - best for accurate information on the applicant's medical history
- Investigative Consumer (Inspection) Report - includes information on an applicant's character, general reputation, personal habits, and mode of living that is obtained through investigation
- MIB report - helps companies share adverse medical information on insured
-
Individual Accident & Health Insurance Policy Provisions
Individual Accident & Health Insurance Policy Provisions in Arkansas for Health InsuranceIndividual Accident And Health Insurance Policy Provisions
TERMS TO KNOW
- Guaranteed renewable: A policy that is written on a noncancellable basis with the right to renew guaranteed
- Irrevocable beneficiary: A beneficiary who has a vested interest in the policy and, therefore, the policyowner may not exercise certain rights without the consent of the beneficiary
- NAIC: National Association of Insurance Commissioners, an organization composed of insurance commissioners from all 50 states, the District of Columbia, and the 5 U.S. territories, formed to resolve insurance regulatory issues
- Total disability: The inability of the insured to perform any occupation for which the insured is reasonably suited by education, training, or experience
- Waiver: Relinquishment of a right or interest
A. Uniform Required Provisions
-
Entire Contract: The health insurance policy, together with a copy of the signed application and attached riders and amendments, constitutes the entire contract. No changes may be made to the policy without the express written agreement of both parties, and any changes must also be made a part of the contract. Only an executive officer of the company, not an agent, has authority to make any changes to the policy.
-
Grace Period: The grace period is the period of time after the premium due date in which premiums may still be paid before the policy lapses for nonpayment of the premium.
-
Reinstatement: If the premium has not been paid by the end of the policy's grace period, the policy will lapse. This provision stipulates under what conditions the insured may reinstate coverage.
-
Change of Beneficiary: The policyowner may change the beneficiary at any time by providing a written request to the insurer. The consent of the beneficiary is not required unless the beneficiary designation is irrevocable.
-
Claims Procedures: This provision spells out the insured's duty to provide the insurer with reasonable notice in the event of a loss. Notice is required within a specified period.
-
Physical Examination and Autopsy: The insurer has the right to examine the insured at its own expense as often as may be reasonably necessary while a claim is pending.
-
Time Limit on Certain Defenses (Incontestable): No statement or misstatement made in the application at the time of issue can be used to deny a claim after the policy has been in force for a certain number of years.
-
Legal Actions: Limits the time during which a claimant may seek recovery from an insurer under a policy.
B. Uniform Optional Provisions
-
Change of Occupation: Allows the insurer to adjust benefits if the insured changes occupations.
-
Misstatement of Age and Sex: Benefits are adjusted if an insurer discovers a misstatement of age on an insurance application.
-
Illegal Occupation: Denies liability if the insured is injured while committing an illegal act or is engaged in an illegal occupation.
-
Intoxicants and Narcotics: The insurer is not liable for any claims that result while the insured is intoxicated or under the influence of drugs.
C. Other Provisions And Clauses
-
Insuring Clause: A general statement that identifies the basic agreement between the insurance company and the insured.
-
Right to Examine (Free Look): Allows the insured a period to review the policy and return it for a full refund if dissatisfied.
-
Consideration Clause: Both parties must give valuable consideration for the contract.
-
Probationary Period: Specifies a waiting period before coverage for specified conditions goes into effect.
-
Elimination Period: A deductible period that must pass before benefits become payable.
-
Coinsurance: Requires sharing of expenses between the insured and the insurance company.
-
Exclusions: Specifies causes of loss that are not covered.
D. Riders
-
Impairment or Exclusions Rider: Excludes coverage for a specified pre-existing condition.
-
Guaranteed Insurability Rider: Allows the insured to purchase additional coverage without evidence of insurability.
E. Rights Of Renewability
-
Noncancellable: The insurer cannot cancel the policy or raise premiums beyond the stated amount.
-
Cancellable: Allows the insurer to cancel the policy with proper notice.
-
Guaranteed Renewable: The insurer can increase premiums on a class basis only, but the insured has the unilateral right to renew the policy.
-
Disability Income and Related Insurance
Disability Income and Related Insurance in Arkansas Health Insurance PoliciesDisability Income And Related Insurance
Disability income insurance is a broad and complex topic. This section will introduce you to some of its basic principles. You will learn about the conditions under which a person can qualify for disability benefits, the specifics of individual and group disability underwriting, and the benefits that are available through the Social Security and Workers Compensation programs. With disability insurance, the key is to understand what injuries qualify for benefits, how much the payments will be, and how long they will last.
TERMS TO KNOW
- Benefit period — a period of time during which benefits are paid under the policy
- Capital sum — a portion of the principal sum of a health insurance policy; paid for accidental dismemberment or loss of sight in one eye
- Earned income — salary, wages, or commissions; but not income from investments, unemployment benefits, and similar sources of income
- Overinsurance — insurance that exceeds in amount the actual value of the person or property insured or insurance in a greater amount than the insured can afford
- Principal sum — the amount of coverage paid for an accidental death under a health insurance policy
- Tax deductible — a qualified expense that may reduce the amount of income subject to taxation
- Taxable — subject to taxation
- Total disability — inability of the insured to perform any occupation for which he or she is reasonably suited by reason of education, training or experience
- Waiver — relinquishment of a right or interest
A. Qualifying For Disability Benefits
One major risk that individuals face in their lifetime is the possibility that they will become totally disabled and be unable to perform work duties for a period of time. Recent statistics show that there is a 30% chance of a 25-year-old being disabled for more than 90 days prior to age 65. It is far less likely that the same 25-year-old will suffer a premature death prior to age 65.
For most people who are unable to go to work, employment income would terminate after a brief period of time. Consequently, most people would be forced to turn to personal savings to pay normal living expenses such as food, rent and utilities. A question to ask is how long a person can survive without any income. Disability income insurance is designed to replace lost income in the event of this contingency, and is a vital component of a comprehensive insurance program. It may be purchased individually or through an employer on a group basis.
Disability income benefits are limited to a percentage of earned income. The insurer wants a claimant to have a financial incentive to return to work. A person becomes eligible for regular disability benefits when they meet the insurance company's definition of disability due to either a sickness or an injury. This definition of disability does vary from company to company. It is important for the applicant and the producer to be fully aware of this important benefit trigger.
- Total Disability
Total disability is defined differently under some disability income policies. Some policies use a relatively strict definition such as the any occupation definition, similar to Social Security. This definition of total disability requires the insured to be unable to perform any occupation for which the insured is reasonably suited by reason of education, training or experience. Other insurers have adopted a more liberal definition that defines total disability as the "inability to perform the duties of one's own occupation." As would be expected, the more liberal "own occupation" definition of disability makes it easier to qualify for disability benefits.
Own Occupation
An own occupation policy will provide benefits when the insured is unable to perform any duties of their own occupation because of sickness or accident. This definition is usually limited to the first 24 months after a loss. It allows insureds (claimants) to receive benefits if, because of disablement, they cannot perform the duties of their normal occupation even though they might be able to earn income from a different occupation. After 24 months, if the insured is still unable to perform the duties of their own occupation, the definition of disability narrows to mean the inability to perform any occupation for which the insured is reasonably suited by education, training, or experience. This is a dramatic reduction in the insurer's liability because it is very likely that claimants can find something they can do for financial gain. The “own occ” definition is generally used for highly trained, skilled occupations such as surgeons, trial attorneys, etc.
Any Occupation
A policy that has an "any occupation" provision will only provide benefits when the insured is unable to perform any of the duties of the occupation for which they are suited by reason of education, training, or experience. "Own occupation" is the more liberal definition and therefore provides a better benefit for the insured. Although some companies still utilize the two-tier approach by combining both definitions in a single disability income policy, from an underwriting standpoint, it is much easier for an insurance company to justify the "any occupation" definition when agreeing to issue a policy.
Know This! Considering a disabled insured is able to perform some duties of the occupation, coverage under the "any occupation" policy is more likely to be denied than under the "own occupation" policy.
- Partial Disability
Partial disability is often defined as the inability to perform one or more of the regular duties of one’s own occupation or the inability to work on a full-time basis, which results in a decrease in the individual's income. The purpose of the partial disability benefit is to cover a partial loss of income when the insured is disabled to the point of being able to report to work, but not being able to perform all of the regular duties of the job. The partial disability benefit is typically 50% of the total disability benefit and is limited to a certain period of time, as noted in the policy.
The benefits paid on a partial disability policy are paid in a flat amount or a residual amount.
Know This! Partial disability covers a partial loss of income for disabled insureds who are unable to perform some, but not all, of their regular job duties.
- Residual Disability
Residual disability is the type of disability income policy that provides benefits for loss of income when a person returns to work after a total disability but is still not able to work as long or at the same level he/she worked before becoming disabled. Many companies have replaced partial disability with residual disability. Residual disability will help pay for loss of earnings. If the person can only work part-time or at a lesser paying position, residual disability will make up the difference between their present earnings and what they were earning prior to disability.
Know This! Residual disability is calculated as a percentage, determined by current earnings and earnings prior to disablement.
- Presumptive Disability
Presumptive Disability is a provision that is found in most disability income policies which specifies the conditions that will automatically qualify the insured for full disability benefits. Some disability policies provide a benefit when people simply meet certain qualifications, regardless of their ability to work. The presumptive disability benefit provides a benefit for dismemberment (the loss of use of any two limbs), total and permanent blindness, or loss of speech or hearing. Some policies require actual severance of limbs rather than loss of use.
- Recurrent Disability
Recurrent Disability is generally expressed in a policy provision that specifies the period of time (usually within 3-6 months), during which the recurrence of an identical or related disability is considered a continuation of the original disability and therefore not subject to a new elimination period. This provision also allows a person who has returned to work to have their benefits re-established if they have a recurrence of the same disability. In the case of a disability resulting from an injury, recurrent disability is defined as the inability to perform one or more duties of the occupation on a part-time or full-time basis.
- Presumptive Disability
Presumptive Disability is a provision that is found in most disability income policies which specifies the conditions that will automatically qualify the insured for full disability benefits. Some disability policies provide a benefit when people simply meet certain qualifications, regardless of their ability to work. The presumptive disability benefit provides a benefit for dismemberment (the loss of use of any two limbs), total and permanent blindness, or loss of speech or hearing. Some policies require actual severance of limbs rather than loss of use.
- Recurrent Disability
Recurrent Disability is generally expressed in a policy provision that specifies the period of time (usually within 3-6 months), during which the recurrence of an identical or related disability is considered a continuation of the original disability and therefore not subject to a new elimination period. This provision also allows a person who has returned to work to have their benefits re-established if they have a recurrence of the same disability. In the case of a disability resulting from an injury, recurrent disability is defined as the inability to perform one or more duties of the occupation on a part-time or full-time basis.
B. Individual And Group Disability Underwriting
Disability underwriting is the process of evaluating the risk of insuring an individual or a group against loss of income caused by injury or sickness. The purpose of underwriting is to maintain profitability for the insurance company, while providing adequate coverage to the insureds. There are many factors that affect this process, and each company has their own guidelines. Generally, the two major types of disability income underwriting are individual and group.
Individual Disability Underwriting
Individual disability insurance is purchased by an individual and is not associated with a group or employer. Each individual has to go through an underwriting process. Underwriting will evaluate an individual's age, gender, occupation, income, overall health, and medical history. In addition, consideration is given to the number of years the individual has been in the occupation. The primary purpose of disability income insurance is to replace lost income. Therefore, an individual’s ability to earn an income is a key consideration when determining eligibility for coverage. Insurers may require a medical examination or request access to medical records to assess an individual's health and determine the risk involved.
Group Disability Underwriting
Group disability insurance is typically offered by an employer as part of an employee benefits package. Underwriting for group disability insurance is based on the characteristics of the group rather than the individual members. Factors such as the average age, gender, occupation, and overall health of the group are considered in group underwriting. Group disability insurance is often less restrictive in terms of medical history and health requirements compared to individual disability insurance.
C. Benefit Availability
The availability of disability benefits can vary depending on the type of policy and the source of coverage. There are several sources of disability benefits, including individual disability insurance, group disability insurance, Social Security Disability Insurance (SSDI), and workers' compensation. It's important to understand the benefits available from each source.
- Individual Disability Insurance
Individual disability insurance provides coverage to individuals who purchase a policy on their own, separate from any group or employer-sponsored coverage. The benefits provided by individual disability insurance can be tailored to the policyholder's specific needs and circumstances. Benefits are typically based on the terms of the policy, including the benefit amount, waiting period (elimination period), and benefit period. Individuals pay premiums for this coverage to ensure financial protection in case of disability.
-
Group Disability Insurance
Group disability insurance is typically offered by employers to their employees as part of an employee benefits package. This coverage is designed to provide income replacement for employees who become disabled and are unable to work. The terms and conditions of group disability insurance are set by the employer and insurance provider, and they can vary widely. Group disability insurance may include short-term disability (STD) and long-term disability (LTD) coverage, with different benefit structures.
-
Social Security Disability Insurance (SSDI)
Social Security Disability Insurance (SSDI) is a federal government program that provides disability benefits to eligible individuals. To qualify for SSDI benefits, individuals must meet specific criteria, including having a disability that is expected to last for at least 12 months or result in death. The Social Security Administration (SSA) administers SSDI, and benefits are based on an individual's earnings history. SSDI provides a safety net for people who have paid into the Social Security system and become disabled.
-
Workers' Compensation
Workers' compensation is a state-based insurance program that provides benefits to workers who are injured or become disabled while on the job. The eligibility criteria and benefits provided by workers' compensation can vary by state, but the program is generally intended to cover medical expenses and lost wages related to work-related injuries and disabilities. Workers' compensation is a form of insurance required by employers to protect their employees in case of work-related accidents.
Know This! While individual and group disability insurance are purchased or provided voluntarily, SSDI and workers' compensation are government-mandated programs that provide benefits to eligible individuals.
Please let me know if you need more specific information or if there are any other questions you have related to disability income insurance and related topics.
E. Business Disability Insurance
Just as an individual purchases disability income insurance to protect his/her ability to earn a living, a business purchases business disability insurance on its key employees to protect it from loss when the employee becomes disabled.
- Key Person Disability
Key person disability is purchased by the employer on the life of a key employee. The key person's economic value to the business is determined in terms of the potential loss of business income which could occur as well as the expense of hiring and training a replacement for the key person. The contract is owned by the business, the premium is paid by the business, and the business is the beneficiary. The person is the insured, and the business must have the key person's consent to be insured in writing.
Know This! In key person disability insurance, the business is the contract owner, premium payor, and the beneficiary.
- Disability Buy-sell Policy
A buy-sell agreement is a legal agreement prepared by an attorney. The buy-sell agreement specifies how the business will pass between owners when one of the owners dies or becomes disabled. It is common for the business to purchase insurance to provide the cash to accomplish the buyout when the owner either dies or becomes disabled. The policies that fund buy-sell agreements generally have an extremely long elimination period, possibly one or two years. Generally, these policies funding buy-sell agreements also provide a large lump-sum benefit to buy out the business rather than monthly benefits.
- Business Overhead Expense Policy
Business overhead expense (BOE) insurance is a unique type of policy that is sold to small business owners who must continue to meet overhead expenses, such as rent, utilities, employee salaries, installment purchases, or leased equipment, following a disability. The business overhead expense policy reimburses the business owner for the actual overhead expenses that are incurred while the business owner is totally disabled. This policy does not reimburse the business owner for their salary, compensation, or other form of income that is lost as a result of disability. There is usually an elimination period of 15 to 30 days, and benefit payments are usually limited to one or two years. The benefits are usually limited to covered expenses incurred or the maximum monthly benefit stated in the policy. The premiums paid for BOE insurance are tax-deductible to the business as a business expense. However, the benefits received are taxable to the business as received.
F. Social Security Disability
Social Security, also referred to as Old Age Survivors Disability Insurance — OASDI, is a federal program enacted in 1935, which is designed to provide protection for eligible workers and their dependents against financial loss due to old age, disability, or death. With a few exceptions, almost all individuals are covered by Social Security. In some respects, Social Security plays a role of federal life and health insurance, which is important to consider when determining an individual's needs for life insurance.
- Qualification for Disability Benefits
Social Security uses the Quarter of Coverage (QC) system to determine whether an individual is qualified for Social Security benefits. The type and amount of benefits are determined by the amount of credits or QCs a worker has earned. Anyone working in jobs covered by Social Security or operating their own business may earn up to a maximum of 4 credits for each year of work. The term fully insured refers to someone who has earned 40 quarters of coverage (the equivalent of 10 years of work), and is therefore entitled to receive Social Security retirement, premium-free Medicare Part A, and survivor benefits. If an individual is entitled to premium-free Medicare Part A, they are automatically eligible for Medicare Part B, but must pay a monthly premium. An individual can attain a currently insured status (or partially insured), and by that qualify for certain benefits if the individual has earned 6 credits (or quarters of coverage) during the 13-quarter period ending with the quarter in which the insured:
- Dies;
- Becomes entitled to disability insurance benefits; or
- Becomes entitled to old-age insurance benefits. For younger workers, the number of quarters required to qualify for the benefits differs by age according to a table established by Social Security.
- Definition of Disability
Assuming that one qualifies for Social Security disability benefits by being fully insured or partially insured, one must then meet Social Security’s definition of disability. Disability, under Social Security, is defined as the inability to engage in any substantially gainful activity by reason of a medically determinable physical or mental impairment that has lasted or is expected to last 12 months or result in an early death. This definition is not as liberal as most definitions of disability found in policies marketed through insurance companies.
- Waiting Period
The waiting, or elimination period for Social Security disability benefits is 5 months. Benefits begin at the beginning of the 6th month and are not retroactive to the beginning of the disability.
G. Chapter Recap
This chapter explained the key concepts and major types of disability income insurance, including group individual, group, and business disability policies. Let's recap the key features for each category:
-
DISABILITY INCOME
- Disability Income Insurance
- Replaces lost income in the event of disability
- Insured must be unable to perform occupational duties
- Presumptive disability – specifies condition that qualifies insured for full disability benefits
- Recurrent disability – specifies the period of time during which the recurrence of an injury or illness will be considered a continuation of a prior disability
- Elimination period – waiting period that lasts from the onset of disability until benefit payments start
- Probationary period – period after the policy starts during which benefits won't be paid for illness-related disabilities
- Benefit period – length of time monthly disability benefit payments last
- Benefit limitations – maximum benefits an insurer is willing to accept for an individual risk; based on a percentage of insured’s past earnings
- Social Insurance Supplement (SIS) or Social Security Riders – supplement or replace benefits payable under Social Security Disability
-
Business Disability
- Buy-Sell Agreement
- Specifies who will purchase a business partner's interest in case of disability
- Key Person Disability
- Covers the potential loss of business income and the expense of hiring and training a replacement for a key person
- Business owns the contract, pays the premium, and is the beneficiary
-
Group Disability
- Short-term disability (STD) - benefit period no longer than 2 years
- Long-term disability (LTD):
- Elimination period may last as long as the benefit period for STD
- Benefit period may last until age 65
- Usually reserved for management employees
-
SOCIAL SECURITY BENEFITS
- Basics
- OASDI - Old Age, Survivors, and Disability Insurance
- Provides disability income benefits
- Individual must meet proper insured status, definition of disability, and waiting period requirements
- Qualifying for Disability Benefits
- Fully insured: 40 quarters of coverage (equivalent of 10 years of work)
- Currently insured: 6 credits during the 13-quarter period
- 5-month waiting period
- Benefits based on PIA
- Basics
-
Medical Plans
Medical Plans in Arkansas Health Insurance PlansA. Medical Plan Concepts
Basic medical expense insurance refers to various essential medical, hospital, and surgical benefits. The early health insurance policies sold after the Great Depression were basic plans, which were offered separately as hospital, medical, and surgical plans. Basic plans were characterized by first-dollar coverage (no deductible) and low dollar limits, which meant they afforded no protection to an individual or family against catastrophic medical expenses that could be financially disastrous.
The broad category of medical expense coverages can provide a wide range of benefits, or policies may be narrowly written and provide only one or two types of coverage.
- Fee-for-service Basis vs. Prepaid Basis
Medical expense plans could be fee-for-service where providers receive a payment for their billed charges for each service provided. Prepaid plans provide medical and hospital benefits in the form of service rather than dollars. In prepaid plans, the providers are compensated regularly whether or not they provide service, but no additional compensation is provided when services are rendered.
- Specified Coverages vs. Comprehensive Care
Specified coverage policies are those insurance policies that limit coverage to one illness or one limiting group of coverages, e.g., cancer policies, prescription drug coverage, dental plans, and other limited coverage plans. These policies are commonly written as a stand-alone individual policy or to complement a traditional fee-for-service Major Medical Expense Policy.
Comprehensive care policies are those plans that provide coverage for most types of medical expenses: a comprehensive package of health care services that typically includes preventive care, routine physicals, immunizations, outpatient services, and hospitalization, such as HMOs.
B. Types Of Medical Plans
Health care insurers (carriers) include stock and mutual insurance companies, Blue Cross/Blue Shield, health maintenance organizations (HMOs), and preferred provider organizations (PPOs). Care is administered not only in the doctors' offices or the hospital but also in surgicenters, urgent care centers, and skilled nursing facilities.
- Basic Hospital, Medical and Surgical Policies
Basic hospital, surgical, and medical policies, and major medical policies are commonly grouped into what are referred to as Medical Expense Insurance. They provide benefits for the cost of medical care that results from accidents or sickness.
The three basic coverages (hospital, surgical, and medical) may be purchased separately or together as a package. These types of coverage are often referred to as first-dollar coverage because they usually do not require the insured to pay a deductible. This differs from Major Medical Expense insurance. However, the basic medical coverages usually have more limited coverage than the Major Medical Policies.
Major Medical Expense insurance functions through reimbursement. The insurance company reimburses the medical service provider for any amount due.
Basic hospital expense coverage: Hospital expense policies cover hospital room and board and miscellaneous hospital expenses, such as lab and x-ray charges, medicines, use of the operating room, and supplies, while the insured is confined in a hospital. There is no deductible, and the limits on room and board are set at a specified dollar amount per day up to a maximum number of days. These limits may not provide for the full amount of hospital room and board charges incurred by the insured. For example, if the hospital expense benefit was $500 per day, and the hospital actually charged $650 per day, the insured would be responsible for the additional $150 per day.
****** There are no deductibles for basic hospital expense coverage.
The miscellaneous hospital expenses normally have a separate limit. This amount, which pays for other miscellaneous expenses associated with a hospital stay, can be expressed either as a multiple of the room and board charge (such as 10 times the room and board charge) or as a flat amount. In addition, the policy may specify a maximum limit for certain types of expenses, such as $100 for drugs or $150 for use of the operating room. As with the room and board charges, the hospital miscellaneous expense limits may not pay for the full amount needed by the insured in the event of a lengthy hospital stay.
Basic medical expense coverage is often referred to as Basic Physicians' Nonsurgical Expense Coverage because it provides coverage for nonsurgical services a physician provides. However, the benefits are usually limited to visits to patients confined in the hospital. Some policies will also pay for office visits. There is no deductible with benefits, but coverage is usually limited to a specific number of visits per day, a limit per visit, or a limit per hospital stay.
In addition to nonsurgical physician’s expenses, basic medical expense coverage can be purchased to cover emergency accident benefits, maternity benefits, mental and nervous disorders, hospice care, home health care, outpatient care, and nurses’ expenses. Regardless of what type of plan or coverage is purchased, these policies usually offer only limited benefits that are subject to time limitations. The insured is often required to pay a considerable sum of money in addition to the benefits paid by the medical expense policies.
Basic surgical expense coverage: This coverage is commonly written in conjunction with Hospital Expense policies. These policies pay for the costs of surgeons’ services, whether the surgery is performed in or out of the hospital. Coverage includes surgeons’ fees, anesthesiologist, and the operating room when it is not covered as a miscellaneous medical item. As with the other types of basic medical expense coverage, there is no deductible, but coverage is limited. Each contract has a surgical schedule that lists the types of operations covered and their assigned dollar amounts. If the operation is not listed, the contract may pay for a comparable operation. Special schedules may express the amount payable as a percentage of the maximum benefit, list a specified amount, or assign a relative value that when multiplied by its conversion factor gives the benefit payable.
When the relative value approach is used, each surgical procedure will be assigned a number of points that are relative to the number of points assigned to the maximum benefit. The maximum points are usually assigned to major surgical procedures, such as open-heart surgery. The points for this maximum benefit are usually high, such as 1,000 points. Other surgical procedures, such as an appendectomy, may only have an assigned point value of 200. In order to determine the amount payable for the appendectomy, the assigned points (relative value) of 200 are multiplied by a conversion factor. This conversion factor represents the total amount payable per point.
For example, if the conversion factor was 10, the policy would pay $2,000 for the appendectomy (200 x 10) and $10,000, the maximum benefit, for the open-heart surgery (1,000 x 10).
- Major Medical Policies
Major Medical expense plans were developed from basic hospital expense policies as a result of the increased sophistication and expense involved with medical procedures and techniques.
Regular basic medical expense policies are characterized by their low dollar limits and first-dollar coverage, but they afforded no protection to an individual or family against catastrophic medical expenses that would be financially disastrous. The Major Medical policy was designed to provide protection against catastrophic loss. By using deductibles and coinsurance, this coverage was made affordable because the policy did not respond to the small claims (those that could be covered under a basic plan, or absorbed by the insured), and provides coverage for the less frequent, but financially disastrous, catastrophic losses.
Characteristics Major medical expense contracts are characterized by high maximum limits, blanket coverage, coinsurance, and a deductible. Dollar deductibles are paid upfront, and the coinsurance, or sharing of the cost, is paid after the deductible is met and the claim is submitted.
Common Limitations Generally, most major medical plans cover most medical expenses in and out of the hospital, and they have high maximum benefit limits. These plans are called covered or eligible expense plans.
Exclusions from Coverage The following are among the exclusions found in major medical insurance policies:
- Injuries caused by war
- Intentionally self-inflicted injuries
- Regular dental/vision/hearing care
- Custodial care
- Injuries covered by workers' compensation insurance
- Cosmetic surgery (unless necessitated by a birth defect or an accident)
Provisions Affecting Cost to Insureds Major medical policy premiums vary depending on the amount of the deductible, the coinsurance percentage, the stop-loss amount, and the maximum amount of the benefit.
Deductibles Most companies incorporate an annual deductible into their major medical policy. A typical deductible could range from $100 to $2,500. The deductible amount is the portion of medical expenses that are paid by the insured each year before the insurance benefits start. The higher the deductible, the lower the annual premium for the coverage will be. In other words, if you accept more risk through a higher deductible, the insurance company lowers your premium.
***** Higher deductible = lower premium.
Stop-loss Feature Many insurance companies include a stop-loss feature in their major medical policies. The stop-loss amount would be the amount that the insured pays out of pocket during the year. When the insured’s out-of-pocket expenses reach the stop-loss, the insurance company then provides coverage at 100% of eligible expenses for the remainder of the year. The out-of-pocket expenses that qualify for the stop-loss would be the insured’s portion of the coinsurance, and it may or may not include the deductible. The higher the stop-loss, the lower the premium will be.
Impairment Rider The impairment (exclusion) rider may be attached to a contract for the purpose of eliminating coverage for a specifically defined pre-existing condition, such as back injuries. Impairment riders may be temporary or may become a permanent part of the policy. Attaching this rider excludes coverage for a condition that would otherwise be covered. Often a person's only means of purchasing insurance at a reasonable cost when they have an existing impairment is through a policy which excludes coverage for the specific impairment.
For example, a physician may have suffered from a back injury prior to applying for a disability policy. The company may agree to issue a disability policy, but with an exclusion rider, excluding coverage for any claim related to his back. The policy would cover any other disability he may incur in the future, as long as it is not related to his back. This may be the only way the insured is able to obtain coverage. The underwriter makes a decision, when writing the contract, whether to make the exclusion permanent, or for a short time only (such as if the insured is able to go a specified period of time with no further treatment). The terms of the rider will be clearly stated in the policy.
Most riders in both life and health insurance add some form of additional coverage and often, there is extra cost added to the premium for the rider. The impairment (exclusion) rider is an exception in that it takes something away from standard coverage. There is no extra charge for this, nor is the premium reduced to reflect a reduction in coverage.
- Health Maintenance Organizations (HMOs)
By means of the Health Maintenance Act of 1973, Congress strongly supported the growth of health maintenance organizations (HMOs) in this country. The act forced employers with more than 25 employees to offer the HMO as an alternative to their regular health plans. (The part of the act requiring dual choice has expired and has not been reenacted).
Preventive Care Services The main goal of the HMO Act was to reduce the cost of health care by utilizing preventive care. While most insurance plans offered no benefits for preventive care prior to 1973, HMOs offer free annual check-ups for the entire family. In this way, the HMOs hope to catch diseases in the earliest stages, when treatment has the greatest chance for success. The HMOs also offer free or low-cost immunizations to members in an effort to prevent certain diseases.
***** The main focus for an HMO is preventive care.
General Characteristics
The HMO provides benefits in the form of services rather than in the form of reimbursement for the services of the physician or hospital. Traditionally, the insurance companies provide the financing, while the doctors and hospitals have provided the care. The HMO concept is unique in that the HMO provides both the financing and patient care for its members.
Limited Service Area The HMO offers services to those living within specific geographic boundaries, such as county lines or city limits. If individuals live within the boundaries, they are eligible to belong to the HMO, but if they do not live within the boundaries, they are ineligible.
Limited Choice of Providers The HMO tries to limit costs by only providing care from physicians that meet their standards and are willing to provide care at a prenegotiated price.
Copayments A copayment is a specific part of the cost of care or a flat dollar amount that must be paid by the member. For example, the member may be required to pay $5, $10, or $25 for each office visit.
There is usually no deductible required under HMO plans.
Prepaid Basis HMOs operate on a capitated basis: the HMO receives a flat amount each month attributed to each member, whether the member sees a physician or not. In essence, it is a prepaid medical plan. As a member of the plan, you will receive all services necessary from the member physicians and hospitals.
Primary Care Physician vs. Referral (Specialty) Physician Care is provided to members of the HMO by a limited number of physicians that are approved to practice in the HMO.
Primary Care Physician (PCP) When an individual becomes a member of the HMO, they will choose their primary care physician (PCP) or gatekeeper. Once chosen, the primary care physician or HMO will be regularly compensated for being responsible for the care of that member, whether care is provided or not. It should be in the primary care physician’s best interest to keep this member healthy to prevent future time for treatment of disease.
Referral (Specialty) Physician In order for the member to get to see a specialist, the primary care physician (gatekeeper) must refer the member. The referral system keeps the member away from higher priced specialists unless it is truly necessary. In many HMOs, there is a financial cost to the primary care physician for referring a patient to the more expensive specialist, thus the primary care physician may be inclined to use an alternative treatment before approving a referral. HMOs must have mechanisms to handle complaints which sometimes result in a delay of referral, or complaints about other patient care or coverage concerns.
Know This! In an HMO, a gatekeeper helps control the cost of healthcare by only making the necessary referrals.
Hospital Services and Emergency Care The HMO provides the member with inpatient hospital care, in or out of the service area. The services may be limited for treatment of mental, emotional or nervous disorders, including alcohol or drug rehabilitation or treatment.
Emergency care must be provided for the member in or out of the HMO's service area. If emergency care is being provided for a member outside the service area, the HMO will make an effort to get the member back into the service area so that care can be provided by salaried member physicians.
- Preferred Provider Organizations (PPOs) The Preferred Provider Organizations (PPOs) could be seen as the traditional medical systems’ answer to HMOs. In the PPO system, the physicians are paid fees for their services rather than a salary, but the member is encouraged to visit approved member physicians that have previously agreed upon the fees to be charged. This encouragement comes in the form of benefits. While the members can utilize any physician they choose, the PPO may provide 90% of the cost of a physician on their approved list while possibly only providing for 70% of the cost if the member chooses to utilize a physician not included on the PPO's approved list.
A PPO is a group of physicians and hospitals that contract with employers, insurers, or third-party organizations to provide medical care services at a reduced fee. The PPOs differ from the HMOs in two ways. First, they do not provide care on a prepaid basis, but physicians are paid a fee for service. Secondly, subscribers are not required to use physicians or facilities that have contracts with the PPO.
*****Unlike HMOs, PPOs allow more flexibility between in-network and out-network providers, in exchange for a higher premium.
Any physician or hospital that qualifies and agrees to follow the PPO’s standards and charge the appropriate fees that the PPO has established can be added to the PPO’s approved list at any time. Physicians and providers may belong to several PPO groups simultaneously.
- Point of Service (POS) Plans The Point-Of-Service (POS) plan is merely a combination of HMO and PPO plans.
Nature and Purpose With the Point-Of-Service plan, employees do not have to be locked into one plan or make a choice between the two plans. A different choice can be made every time a need arises for medical services.
Out-of-network Provider Access PPO plans, like HMOs, enter into contractual arrangements with healthcare providers who form a provider network. However, plan members do not have to use only in-network providers for their care.
Similarly, in a POS plan, individuals can visit an in-network provider at their discretion. If they decide to use an out-of-network physician, they may do so. However, the member copays, coinsurance, and deductibles may be substantially higher.
In POS plans, participants usually have access to a provider network that is controlled by a primary care physician ("gatekeeping"). Plan members, however, have an option to seek care outside the network, but at reduced coverage levels.
POS plans are also referred to as "open-ended HMOs."
PCP Referral (Gatekeeper PPO) In a PPO, the insured does not have to select a primary care physician. The insured may choose medical providers not found on the preferred list and still retain coverage. The insured is allowed to receive care from any provider, but if the insured selects a PPO provider, the insured will pay lower out-of-pocket costs. If an out-of-network provider is used, the insured's out-of-pocket costs will be higher. In a PPO, all network providers are considered "preferred," and insureds can visit any of them, even specialists, without first seeing a primary care physician. Certain services may require plan pre-certification, an evaluation of the medical necessity of inpatient admissions and the number of days required to treat a physical condition.
Know This! In-network provider = lower out-of-pocket costs; out-of-network provider = higher out-of-pocket costs.
Indemnity Plan Features If a non-member physician is utilized under the Point-Of-Service plan, then the attending physician will be paid a fee for service, but the member patient will have to pay a higher coinsurance amount or percentage for the privilege.
C. Limited Health Insurance Policies
There are a variety of health insurance policies providing limited coverage for specific accidents or sickness. These contracts must specify the type of accident or sickness covered, limited perils, and amounts of coverage. Benefits may be paid on an expense-paid (reimbursement) basis or indemnity basis.
Know This! Limited policies cover a specific sickness or accident only.
- Short-Term Medical
Short-term medical insurance plans are designed to provide temporary coverage for people in transition (those between jobs or early retirees) and are available for terms from one month up to 11 months, depending on the state. Unlike regular individual major medical plans, short-term health insurance policies are not regulated by the Affordable Care Act, and their enrollment is not limited to the open enrollment period; they also do not meet the requirements of the federally mandated health insurance coverage.
Like traditional health plans, short-term plans may have medical provider networks, and impose premiums, deductibles, coinsurance, and benefit maximums. They also cover physician services, surgery, outpatient and inpatient care.
- Accident
Accident-only policies are limited policies that provide coverage for death, dismemberment, disability, or hospital and medical care resulting from an accident. Because it is a limited medical expense policy, it will only pay for losses resulting from accidents and not sickness.
- Accidental Death and Dismemberment
Accidental Death and Dismemberment (AD&D) coverage can be written as a rider or as a separate policy. However, most frequently, it is part of group life and group health plans. It provides for the payment of a lump-sum benefit in the event that the insured dies from an accident, as defined in the policy, or in the event of the loss of certain body parts caused by an accident.
Accidental Death and Dismemberment coverage only pays for accidental losses and is thus considered a pure form of accident insurance. The principal sum is paid for accidental death. This amount is usually equal to the amount of coverage under the insurance contract, or the face amount. In case of the loss of sight or accidental dismemberment, a percentage of that principal sum will be paid by the policy, often referred to as the capital sum. The amount of the benefit will vary according to the severity of the injury.
The policy will usually pay the full principal for the loss of sight in both eyes or the loss of two or more limbs; however, it may only pay 50% for the loss of one hand or one foot. In addition, some policies will pay double or triple indemnity, meaning the policy will pay twice or three times the face amount in the event of accidental death.
Most policies will pay the accidental death benefit as long as the death is caused by the accident and occurs within 90 days.
Know This! In AD&D policies, the principal sum means the full face amount (100%), and the capital sum is a percentage of the face amount.
There are also two special policies that pay accidental death and dismemberment benefits only under specific circumstances, Limited Risk Policies, and Special Risk Policies. The Limited Risk Policy defines the specific risk in which accidental death or dismemberment benefits will be paid. For example, the policy may be a Travel Accident Policy, in which the benefits are only payable if the loss occurs as a result of travel.
The Special Risk Policy, on the other hand, will cover unusual types of risks that are not normally covered under AD&D policies. It covers only the specific hazard or risk identified in the policy, such as a racecar driver test-driving a new car.
- Critical Illness or Specified Disease
A critical illness policy covers multiple illnesses, such as heart attack, stroke, renal failure, and pays a lump-sum benefit to the insured upon the diagnosis (and survival) of any of the illnesses covered by the policy. The policy usually specifies a minimum number of days the insured must survive after the illness was first diagnosed.
- Hospital Indemnity Plans
A hospital indemnity policy provides a specific amount on a daily, weekly, or monthly basis while the insured is confined to a hospital. Payment under this type of policy is unrelated to the medical expense incurred but is based only on the number of days confined in a hospital. This can also be called a hospital fixed-rate policy.
- Dental Plans
Dental expense insurance is a form of medical expense health insurance that covers the treatment, care, and prevention of dental disease and injury to the insured's teeth. An important feature of a dental insurance plan, which is typically not found in a medical expense insurance plan, is the inclusion of diagnostic and preventive care (teeth cleaning, fluoride treatment, etc.). Some dental plans require periodic examinations as a condition for continued coverage.
Dental expense may be packaged or integrated with other health insurance benefits like major medical. In that case, the integrated plan may have a common deductible. On the other hand, some integrated plans maintain separate deductibles for the medical and dental portions of the contract.
Pediatric dental coverage is an essential health benefit under the Affordable Care Act that must be available as part of a health plan or as a stand-alone plan for children 18 or younger. However, insurers do not have to offer adult dental coverage.
Depending on the state, pediatric dental benefits may be offered through one of the following types of plans:
A qualified health plan that includes dental coverage;
A stand-alone dental plan purchased in conjunction with a qualified health plan; or
A contracted/bundled plan.
Know This! Health insurers must offer pediatric dental coverage (for children 18 or younger) as an essential health benefit under a health plan or as a stand-alone dental plan.
- Vision and Hearing Plans
Some employers provide this form of group health insurance to their employees to cover eye examinations and eyeglasses or hearing aids on a limited basis.
Know that per the Affordable Care Act, pediatric vision benefits are mandatory.
It is common in most vision expense insurance plans to restrict benefits to one exam and one pair of glasses in any 12-month period.
D. Cost Containment In Health Care Delivery
With the dramatic rise in the cost of medical care over the past few decades, the concept of managed care has become a necessity for insurance companies.
Managed care plans, such as HMOs and PPOs, are designed to control costs by controlling the behavior of the plan participants.
- Cost-saving Services
Cost-saving services or case-management provisions provide plans with controlled access to providers, large claim management, preventive care, hospitalization alternatives, second surgical opinions, preadmission testing, catastrophic case management, risk sharing, and providing high quality of care.
Insurance companies use the services of case managers for large, ongoing claims through a process of utilization management. The case manager evaluates the appropriateness, necessity, and quality of health care, and may include prospective and concurrent review.
Preventive Care
Managed care plans encourage preventive care and living a healthier lifestyle. Annual physical exams, mammograms, and other procedures used to detect medical problems before symptoms appear can result in considerable cost savings if a problem is detected early and treated quickly.
Hospital Outpatient Benefits
Because hospital confinement has become so costly, many plans require the patient to take advantage of outpatient services when possible.
Alternatives to Hospital Services
Alternatives to hospital care might include home health care where the patient stays at home and is visited periodically by a health professional. A home health aide that could work in conjunction with a family member may meet daily needs. Terminally ill patients may elect hospice care rather than a hospital stay. Hospice attends to the patient’s daily needs and provides pain relief but attempts no curative procedures. Within cost containment, painkillers and special hospital beds are paid for, but operations or antibiotics are not.
Managed Care
Managed care plans’ main characteristic is that they try to contain costs of health care services while providing efficient services. Strategies used by managed care plans are:
- Providing financial incentives for members to use providers and procedures approved by the plan;
- Controlling lengths of hospital stay;
- Using utilization reviews to improve case management;
- Focus on preventive health care.
HMO and PPO plans are some of the examples of managed care plans.
Preauthorization and Second Opinion
Preauthorization is a cost-containment measure requiring that the insured obtain approval from the insurer before getting an expensive surgery, referred to a specialist, or nonemergency healthcare service.
A second opinion is a separate assessment of a patient by a different medical professional who will then affirm or modify the patient's diagnosis and treatment plan.
- Utilization Management
Utilization management is a system for reviewing the appropriateness and efficient allocation of health care services and resources that are being given or are proposed to be given to an insured. It also covers the review of claims for services that may be covered by a health care provider. There are different types of utilization management reviews: prospective, retrospective, and concurrent review.
Prospective Review
Under the prospective review or precertification process, the physician can submit claim information prior to providing treatment to know in advance if the procedure is covered under the insured’s plan and at what rate it will be paid.
Concurrent Review
Under the concurrent review process, the insurance company will monitor the insured’s hospital stay to make sure that everything is proceeding according to schedule, and that the insured will be released from the hospital as planned.
E. HIPAA (Health Insurance Portability And Accountability Act) Requirements
Legislation that took effect in July 1997 ensures "portability" of group insurance coverage and includes various required benefits that affect small employers, the self-employed, pregnant women, and the mentally ill. HIPAA (Health Insurance Portability and Accountability Act) regulates protection for both group health plans (for employers with 2 or more employees) and for individual insurance policies sold by insurance companies.
HIPAA includes the following protections for coverage:
Group Health Plans:
- Prohibiting discrimination against employees and dependents based on their health condition; and
- Allowing opportunities to enroll in a new plan to individuals in special circumstances.
Individual Policies:
- Guaranteeing access to individual policies for qualifying individuals; and
- Guaranteeing renewability of individual policies.
- Eligibility
HIPAA has regulations regarding eligibility for employer-sponsored group health plans. These plans cannot establish eligibility rules for enrollment under the plan that discriminate based on any health factor relating to an eligible individual or the individual's dependents. A health factor includes any of the following:
- Health status;
- Medical conditions (both physical and mental);
- Claims experience;
- Receipt of health care;
- Medical history;
- Genetic information;
- Disability; or
- Evidence of insurability, which includes conditions arising out of acts of domestic violence and participation in such activities as motorcycling, skiing, or snowmobiling.
Employer-sponsored group health plans may apply waiting periods prior to enrollment as long as they are applied uniformly to all participants.
To be eligible under HIPAA regulations to convert health insurance coverage from a group plan to an individual policy, an individual must meet the following criteria:
- Have 18 months of continuous creditable health coverage;
- Have been covered under a group plan in most recent insurance;
- Have used up any COBRA or state continuation coverage;
- Not be eligible for Medicare or Medicaid;
- Not have any other health insurance; and
- Apply for individual health insurance within 63 days of losing prior coverage.
Such HIPAA-eligible individuals are guaranteed the right to purchase individual coverage.
- Guaranteed Issue
If the new employee meets the requirements, the employer must offer coverage on a guaranteed issue basis.
- Renewability
At the plan sponsor's option, the issuer offering group health coverage must renew or continue in force the current coverage. However, the group health coverage may be discontinued or nonrenewed because of nonpayment of premium, fraud, violation of participation or contribution rules, discontinuation of that particular coverage, or movement outside the service area or association membership cessation.
- Privacy
Under the Privacy Rule for HIPAA (Health Insurance Portability and Accountability Act), protected information includes all "individually identifiable health information" held or transmitted by a covered entity or its business associate, in any form or media, whether electronic, paper, or oral. This is called protected health information (PHI).
Individually identifiable health information includes demographic data that relates to past, present, or future physical or mental health or condition, or payment information that could easily identify the individual.
A covered entity must obtain the individual's written authorization to disclose information that is not for treatment, payment, or health care operations.
F. Affordable Care Act (ACA) The Patient Protection and Affordable Care Act (PPACA), or the Affordable Care Act (ACA), for short, was signed into law on March 23, 2010, as part of the Health Care and Education Reconciliation Act of 2010, to be implemented in phases until fully effective in 2018. Since the bill is a federal law, state regulations are superseded by the PPACA and must conform accordingly.
The Affordable Care Act has mandated increased preventive, educational, and community-based health care services, and was designed to do the following:
- Set up a new competitive private health insurance market.
- Hold insurance companies accountable by keeping premiums low, preventing denials of care, and allowing applicants with pre-existing conditions to obtain coverage (pre-existing conditions exclusions have been eliminated as of January 2014).
- Help stabilize budget and the economy through reducing the deficit by cutting government overspending.
- Extend coverage for adult children in both individual and group health plans until age 26.
In addition, it gives small businesses and nonprofits a tax credit for an employer's contribution to health insurance for employees. It prohibits insurance companies from rescinding health coverage when an insured becomes ill, and eliminates lifetime benefit limits.
Specific health coverage plans, such as retiree-only, stand-alone dental plans, Medigap, and long-term care insurance, are generally exempt from the PPACA changes.
Because these provisions are controversial and health care laws are being challenged in the courts, agents should review current laws to be certain they are giving up-to-date advice.
Eligibility: The Health Insurance Marketplace makes health coverage available to any uninsured individuals. To be eligible for health coverage through the Marketplace, the individual
- Must be a U.S. citizen or national or be lawfully present in the United States;
- Must live in the United States; and
- Cannot be currently incarcerated.
If an individual has Medicare coverage, that individual is not eligible to use the Marketplace to buy a health or dental plan.
Health status (no discrimination): A group health plan or a health insurance issuer offering group or individual health insurance coverage may not establish rules for eligibility based on any of the following health status-related factors related to individuals or their dependents:
- Health status;
- Medical condition (including both physical and mental illnesses);
- Claims experience;
- Receipt of health care;
- Medical history;
- Genetic information;
- Evidence of insurability (including conditions arising out of acts of domestic violence);
- Disability; or
- Any other health status related factor.
When health insurers set their premium rates, they are only permitted to base those rates on 4 standards:
- Geographic rating area (location of residence within the state);
- Family composition (single or family enrollment);
- Age; and
- Tobacco use.
For individual plans, the location is the insured's home address; for small group plans, the location is the employer's principal place of business.
Essential benefits: Essential benefits include hospitalization, maternity, emergency services, wellness and preventive services, and chronic disease management.
Note that all Health Insurance Marketplace plans must cover pregnancy and childbirth, even if pregnancy begins before the coverage takes effect.
Guaranteed issue: Insurance companies must accept any eligible applicant for individual or group insurance coverage. Enrollment for coverage may be restricted to open or special enrollment periods.
Guaranteed renewability: An insurance company that offers either group or individual health insurance coverage must renew or continue the policy at the option of the plan sponsor or the individual.
Pre-existing conditions: The law creates a new program, the Pre-Existing Condition Insurance Plan, to make health coverage available to individuals who have been denied health insurance by private insurance companies because of a pre-existing condition.
Appeal rights: If an insurer rescinds individual or group coverage for reasons of fraud or an intentional misrepresentation of material facts by the insured, the insurer must provide at least 30 days' advance notice to allow the insured time to appeal. An enrollee or insured has the right to review their file, to present evidence and testimony as part of the appeal process, and to keep their coverage in force pending the outcomes of the appeals process.
Coverage for children of the insured: The law extends coverage for children of the insured to age 26 regardless of their marital status, residency, financial dependence on their parents, or eligibility to enroll in their employer's plan.
Coverage for dependent children may continue beyond the limiting age (the child's 26th birthday) if the child continues to be:
- Incapable of self-sustaining employment because of an intellectual or physical disability; and
- Chiefly dependent upon the policyholder or subscriber for support and maintenance.
Lifetime and annual limits: Health plans are restricted from applying a dollar limit on essential benefits, nor can they establish a dollar limit on the amount of benefits paid during the course of an insured's lifetime.
Emergency care: Emergency services must be covered, even at an out-of-network provider, for amounts that would have been paid to an in-network provider for the same services.
Preventive benefits: The ACA requires that 100% of preventive care be covered without cost sharing. Preventive care includes routine checkups, screenings, and counseling to prevent health problems.
Cost-sharing under Group Health Plans: A group health plan must ensure that any annual cost-sharing imposed does not exceed provided limitations.
The ACA has established insurance exchanges that will administer health insurance subsidies and facilitate enrollment in private health insurance, Medicaid, and the Children's Health Insurance Program (CHIP). An exchange can help the applicant to do the following:
- Compare private health plans;
- Obtain information about health coverage options to make educated decisions;
- Obtain information about eligibility or tax credits for the most affordable coverage; and
- Enroll in a health plan that meets the applicant's needs.
Know This! Children of an insured must be covered under the parent's health plan until age 26.
Know This! The Affordable Care Act (ACA) requires all individual and group health insurance plans be issued on a guaranteed issue basis.
1. Essential Health Benefits As mandated by the Affordable Care Act, all private health insurance plans offered in the Marketplace must provide the same set of essential health benefits. All health care plans must include at least the following 10 essential benefits:
- Ambulatory patient services;
- Emergency services;
- Hospitalization;
- Pregnancy, maternity and newborn care;
- Mental health and substance use disorder services, including behavioral health treatment;
- Prescription drugs;
- Rehabilitative and habilitative services and devices;
- Laboratory services;
- Preventive and wellness services and chronic disease management; and
- Pediatric services, including oral and vision care.
2. Levels of Coverage (Metal Plans) Under PPACA, plans are classified into 5 categories of coverage in the Marketplace: four "metal level" plans and catastrophic plans. The metal level plans pay different amounts of the total costs of an average person's care. The actual percentage the insured will pay in total or per service will depend on the services used during the year. On average, the metal level plans will pay as follows:
- Bronze: 60%
- Silver: 70%
- Gold: 80%
- Platinum: 90%
Under the bronze plan, for example, the health plan is expected to cover 60% of the
-
Group Health Insurance
Group Health Insurance in Arkansas by LawGroup Health Insurance
Now that you have examined the different types of health plans, you can further focus on health plans available in group insurance. In this section, you will learn about characteristics of group health insurance, eligibility factors, and provisions that apply exclusively to group coverage. You will also learn about small employer group medical plans and marketing considerations for health insurance providers.
TERMS TO KNOW
- Creditor — a lender of funds
- Debtor — a borrower of funds
- Extension of Benefits — a provision that allows coverage to continue beyond the policy's expiration date for employees who are not actively at work due to disability or who have dependents hospitalized on that date (coverage continues only until the employee returns to work or the dependent leaves the hospital)
- HIPAA — The Health Insurance Portability and Accountability Act is a federal law that protects health information
- Persistency — the tendency or likelihood of insurance policies not lapsing or being replaced with insurance from another insurer
- Self-funded programs — a noninsured plan that uses a trust fund to pay for employees' health care expenses directly
- Underwriting — risk selection and classification process
A. Characteristics Of Group Insurance
In a group policy, the contract is between the insurance company and the group sponsor (the employer, union, trust, or other sponsoring organization), as opposed to the individual policy, where the contract is between the insurance company and the insured.
1. Group Contract
In group insurance, the policy is called the master policy and is issued to the policyowner, which could be the employer, an association, a union, or a trust.
2. Certificate of Coverage
The individuals covered under a group insurance plan are issued evidence of coverage in the form of certificates of insurance, or certificates of coverage. The certificate of insurance cannot contain provisions or statements that are unfair, misleading, or deceptive. The certificate tells what is covered in the policy, how to file a claim, how long the coverage will last, and how to convert the policy to an individual policy.
Know This! The policyowner (employer) receives the master policy; each insured receives a certificate of insurance.
3. Contributory vs. Noncontributory
The same as group life insurance, group health insurance may be either contributory or noncontributory. With a contributory plan, the eligible employees contribute to the payment of the premium (both the employee and employer pay part of the premium). If a plan is contributory, at least 75% of all eligible employees must participate in the plan. If the plan is noncontributory, 100% of the eligible employees must be included, and the participants do not pay part of the premium. The employer pays the entire premium. The reason for these participation requirements is to guard the insurer against adverse selection and to reduce administrative costs.
B. Types Of Eligible Groups
In order to qualify for group coverage, the group must be formed for a purpose other than obtaining group health insurance. In other words, the coverage must be incidental to the group. There are generally 2 types of groups eligible for group insurance: employer-sponsored and association-sponsored.
1. Employment-related Groups
With an employer-sponsored group, the employer (a partnership, corporation, or a sole proprietorship) provides group coverage to its employees. Eligible employees usually must meet certain time-of-service requirements and work full-time. The same as group life insurance, group health insurance may be either contributory or noncontributory.
Individual Employer Plans
The individual employer normally will provide insurance coverage to all full-time employees. The employer can specify within some limitations how many hours are considered full time, and whether both salaried and hourly employees will be covered. The employer can legally exclude a particular group of employees, like union or part-time, from the eligible class of employees.
Multi-Employer Trusts (METs) or Welfare Arrangements (MEWAs)
A Multiple-Employer Trust (MET) is made up of two or more employers in similar or related businesses who do not qualify for group insurance on their own. Before HIPAA defined small employers, many small companies were unable to get health insurance at a reasonable cost due to the fact that there weren't enough people in the company to insure. In situations like this, several small companies banded together to create a large pool of people so that the insurance company will provide coverage. This group of employers jointly purchases a single benefits plan to cover employees of each separate employer.
A noninsured plan may operate without the services and funds of an insurance company. Once the trust fund is established, it can pay for employees' health care expenses directly (self-funding). The trustee has charge of the funds, and all financial activities occur through it. As with any self-funded program, the employer assumes legal responsibility for providing coverage, and the employee has no conversion right upon leaving the group coverage.
Multiple Employer Welfare Associations (MEWAs) can be any entity, other than a duly admitted insurer, that establishes an employee benefit plan for the purpose of offering or providing accident and sickness or death benefits to the employees of at least 2 employers, including self-employed individuals and their dependents. A Multiple-Employer Welfare Arrangement (MEWA) is similar to an MET, except that MEWAs are groups of employers that pool their risks in order to self-insure. These groups could be sponsored by an insurance company or an independent administrator who may help a MEWA to design a plan or handle the administration. Groups can be from the same or related industries because of the law of large numbers/similar risks.
Today, the terms have become blurred, and MEWAs and METs are generally known as interchangeable plans. They are considered risky if not fully insured. Some METs/MEWAs are only partially insured, and the individuals or employers retain full responsibility for any debt if not fully insured.
2. Customer Groups (Depositors, Creditor-debtor, Other)
Creditor group insurance, also called credit life and credit disability income insurance, is a specialized use of group life and group health insurance that covers debtors (borrowers). It protects the lending institution from losing money as the result of a borrower’s death or disability. The contract owner is the creditor, such as a bank, a small-loan company, or a credit union. Generally, the debtor is the premium payor, but the lending institution is the beneficiary of the policy. If the debtor dies or becomes disabled, the insurance proceeds are paid to the creditor to liquidate the indebtedness. The amount of insurance cannot exceed the amount of indebtedness.
C. Employer Group Health Insurance
The majority of all health insurance in force today is provided on a group basis. The cost of group health insurance is lower than the cost for individual coverage since the administrative costs and selling expenses found in group health insurance are far less.
Know This! Group health plans typically cost less than individual plans.
1. Insurer Underwriting Criteria
Generally underwriting for group health insurance is similar to underwriting for individual health insurance coverage, but the underwriter evaluates the group as a whole rather than each individual member. The group’s risk profile determines whether the group will be accepted or rejected. As with any type of underwriting, the underwriter tries to avoid adverse selection. Adverse selection describes the tendency of poorer risks seeking out insurance protection.
Group underwriting criteria help insurers determine the acceptability and premium to be charged, and to minimize the possibility of adverse selection. The following are considered in group health insurance underwriting:
- Certificates are guaranteed issue with no individual underwriting;
- Premiums are determined by age, sex, and occupation of the entire group;
- The reasons for forming the group are other than purchasing insurance;
- A certain participation level must be maintained;
- There is a flow of new members through the group; and
- There is an automatic determination of benefits which is not discriminatory (everyone has the same coverage).
Characteristics of Group
One of the differences between group underwriting and individual underwriting is that in groups of 50 or more, medical information cannot be required of plan participants. In small groups, even one bad risk can have an impact on the claims experience of the group. That’s why in some states, insurers may allow some individual underwriting in small groups they insure.
2. Eligibility for Coverage
Group health plans commonly impose a set of eligibility requirements that must be met before an individual member is eligible to participate in the group plan. It is common that in order to be eligible, the employee must be full time (usually 30 hours per week) and have been employed by the employer from 1 to 3 months.
Employee Eligibility
Employer group health insurance generally requires that to be eligible for coverage an employee must be a full-time employee, working in a covered classification, and must be actively at work.
Under the Affordable Care Act (ACA), employers must extend coverage to all employees who work more than 30 hours per week. In addition, small and large employers may not be denied coverage for failure to satisfy the minimum participation or contribution requirements.
Dependent Eligibility
Employer group health insurance generally requires a dependent of an employee to be:
- A spouse;
- A child younger than the limiting age, including natural children of the insured, stepchildren, children legally placed for adoption, and legally adopted children; and/or
- Disabled children who are incapable of self-support because of a physical or mental disability and are dependent upon the insured for support and maintenance.
Most insurers cover domestic or same-sex partners whether or not a state has a domestic partner or civil union law.
Annual Open Enrollment
A 30-day open-enrollment period is available once a year to employees who reject coverage during the initial enrollment period and later wish to have coverage or to add dependent coverage. Evidence of insurability is not required during the open-enrollment period.
Know This! Evidence of insurability is NOT required during the annual open-enrollment period in group policies.
Probationary Period
If an employee/dependent applies for coverage after the open-enrollment period, they may have to satisfy a probationary period and/or prove insurability.
3. Coordination of Benefits Provision
The purpose of the coordination of benefits (COB) provision, found only in group health plans, is to avoid duplication of benefit payments and overinsurance when an individual is covered under multiple group health insurance plans. This provision limits the total amount of claims paid from all insurers covering the patient to no more than the total allowable medical expenses.
The COB provision establishes which plan is the primary plan, or the plan that is responsible for providing the full benefit amounts as it specifies. Once the primary plan has paid its full promised benefit, the insured submits the claim to the secondary, or excess, provider for any additional benefits payable (including deductibles and coinsurance). In no case will the total amount the insured receives exceed the costs incurred or the total maximum benefits available under all plans.
Loss - Amount covered by Primary Plan = Amount covered by Secondary Plan
If all policies have a COB provision, the order of payments is determined as follows:
- If a married couple both have group coverage in which they are each named as dependents on the other's policy, then the person’s own group coverage will be considered primary. The secondary coverage (the spouses' coverage) will pick up where the first policy left off.
- If both parents name their children as dependents under their group policies, then the order of payment will usually be determined by the birthday rule, i.e., the coverage of the parent whose birthday is earlier in the year will be considered primary. Occasionally, the gender rule may also apply, according to which the father's coverage is considered primary.
- If the parents are divorced or separated, the policy of the parent who has custody of the children will be considered primary.
Know This! Coordination of benefits provision ensures that benefits are not paid in excess of the total losses incurred.
4. COBRA
The Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) requires any employer with 20 or more employees to extend group health coverage to terminated employees and their families after a qualifying event. Qualifying events include the following:
- Voluntary termination of employment;
- Termination of employment for reasons other than gross misconduct (e.g. company downsizing); and
- Employment status change: from full time to part time.
For any of these qualifying events, coverage is extended up to 18 months. The terminated employee must exercise extension of benefits under COBRA within 60 days of separation from employment. The employer is permitted to collect a premium from the terminated employee at a rate of no more than 102% of the individual’s group premium rate. The 2% charge is to cover the employer’s administrative costs.
For events such as death of the employee, divorce or legal separation, the period is 36 months for the dependents.
It is important to remember that COBRA benefits apply to group health insurance, not group life insurance. In addition, unlike the conversion privilege in which the individual converts coverage to an individual health insurance policy, COBRA continues the same group coverage the employee had, and the employee pays the group premium that the employer paid (or employer and employee paid if the plan was contributory).
Note that under the Patient Protection and Affordable Care Act, coverage for children of the insured must extend until the adult child reaches the age of 26 (unless the child qualifies as a disabled dependent). The same age limit applies to COBRA coverage for eligible children of the insured. In addition, in the event of loss of dependent child status under the group plan, the dependent child qualifies for a maximum period of continuation coverage of 36 months.
There are also several disqualifying events under which the COBRA benefits may be discontinued. These include failure to make a premium payment, becoming covered under another group plan, becoming eligible for Medicare, or if the employer terminates all group health plans.
Know This! Coverage for dependents under COBRA may be extended to 36 months in the event of the employee's divorce or death.
5. Conversion of Coverage
Terminated employees are permitted to convert their group health coverage to individual insurance without evidence of insurability if the termination was voluntary or involuntary, except for termination due to gross misconduct. This option must be initiated during the conversion period, which is within 31 days of termination of employment. The insurer is allowed to evaluate the individual to determine the appropriate premium, either standard or substandard, but they may not deny coverage based on this evaluation. The converted policy neither needs to provide the same benefits as the group, nor will it have the same premium. The premium for an individual policy usually will be higher.
Know This! If failed to initiate conversion to individual coverage within 31 days, a terminated employee must undergo a new individual approval process, which may require a medical exam.
D. Chapter Recap
This chapter explained the key principles of group health insurance. Let's recap some of the important points:
GROUP INSURANCE
Characteristics of Group Insurance
- Group formed for a purpose other than obtaining group health insurance.
- Master policy - issued to the group sponsor.
- Certificates of insurance - evidence of coverage for the insureds.
- Experience rating: premium based on group as a whole.
- Community rating: premium based on insurer claims experience.
Types of Eligible Groups
- Employer sponsored - individual or Multiple Employer Trust (MET).
- Association - alumni or professional.
Marketing Consideration
- Advertising - truthful and not misleading.
- Jurisdiction - coverage for more than one state; approved in issuing state.
Underwriting
- Every eligible member of the group must be covered regardless of physical condition, age, sex, or occupation.
- Evidence of insurability generally not required.
- 30-day open enrollment period.
- Probationary employees must work a total of 30 hours per week.
Provisions
- Conversion to individual coverage - within 31 days without evidence of insurability.
- Coordination of benefits.
- Change of insurers - carryover of coinsurance and deductibles.
COBRA
Qualifying Events
- Voluntary termination of employment.
- Termination of employment for reasons other than gross misconduct (e.g. company downsizing).
- Employment status change: from full time to part time.
Length of coverage
- 18 months – after qualifying event.
- 36 months – for dependents after events such as death of the employee, divorce, or legal separation.
-
Specialized Health Insurance for Qualified Individuals
Specialized Health Insurance for Qualified Individuals in ArkansasSpecialized Health Insurance For Qualified Individuals
This section will discuss social insurance and its government-sponsored programs of Medicare, Medicaid, and Social Security. You will learn about eligibility requirements, basic benefits, and services provided by each. This section is full of medical terms, acronyms, and numbers. Note that the dollar amounts for different types of Medicare deductibles change frequently, and are provided as reference only. What’s important for you to remember is who qualifies for each type of plan, and what type of coverage they can expect.
TERMS TO KNOW Benefit period — a period of time during which benefits are paid under the policy Enrollee — a person enrolled in a health insurance plan, an insured (doesn't include dependents of the insured) Pre-existing conditions — conditions for which the insured has received diagnosis, advice, care, or treatment during a specific time period prior to the application for health coverage Premium — the money paid to the insurance company for the insurance coverage Social Security Disability Insured Status — fully insured or currently insured, depending on the number of coverage credits earned Waiting period — a period of time that must pass after a loss occurs before the insurer starts paying policy benefits
A. Medicare Medicare is a federal medical expense insurance program for people age 65 and older even if the individual continues to work. Medicare benefits are also available to anyone, regardless of age, who has been entitled to Social Security disability income benefits for 2 years or has permanent kidney failure (End Stage Renal Disease — ESRD).
Persons age 65 years or older who are recent green card holders (permanent residents) or new immigrants to the U.S. and never worked in the U.S. may not immediately qualify for Medicare. If they don't qualify for free Medicare, they can still purchase it if the following eligibility requirements are met:
- Are 65 years of age or older;
- Have recently become a U.S. citizen by naturalization and haven't worked enough quarters to have social security coverage; and
- Are lawfully admitted aliens (green card holders) who have constantly lived in the United States for 5 years or longer and don't qualify for the Social Security benefits.
Medicare is administered by The Center for Medicare and Medicaid Services (CMS), which is a division of the United States Department of Health and Human Services. Medicare is divided into 4 parts:
- Part A (Hospital Insurance) is financed through a portion of the payroll tax (FICA);
- Part B (Medical Insurance) is financed from monthly premiums paid by insureds and from the general revenues of the federal government;
- Part C (Medicare Advantage) allows people to receive all of their health care services through available provider organizations; and
- Part D (Prescription Drugs) is for prescription drug coverage.
Note, however, that the term Original Medicare refers to Part A - Hospital Insurance, and Part B - Medical Insurance only. It covers health care from any doctor, health care provider, hospital, or facility that accepts Medicare patients. It usually does not cover prescription drugs. Original Medicare does not require the patient to choose a primary care doctor, nor does it require a referral to see a specialist, as long as the specialist is enrolled in Medicare.
Know This! Part A is hospital insurance; Part B is medical insurance.
The following are claims terminology and other key terms applicable to Medicare:
- Actual Charge — The amount a physician or supplier actually bills for a particular service or supply.
- Ambulatory Surgical Services — Care that is provided at an ambulatory center. These are surgical services performed at a center that do not require a hospital stay, unlike inpatient hospital surgery.
- Approved Amount — The amount Medicare determines to be reasonable for a service that is covered under Part B of Medicare.
- Assignment — The physician or a medical supplier agrees to accept the Medicare-approved amount as full payment for the covered services.
- Carriers — Organizations that process claims that are submitted by doctors and suppliers under Medicare.
- Coinsurance — The portion of Medicare’s approved amount that the beneficiary is responsible for paying.
- Comprehensive Outpatient Rehabilitation Facility Services — Outpatient services received from a Medicare participating comprehensive outpatient rehabilitation facility.
- Deductible — The amount of expense a beneficiary must first incur before Medicare begins payment for covered services.
- Durable Medical Equipment — Medical equipment such as oxygen equipment, wheelchairs, and other medically necessary equipment that a doctor prescribes for use in the home.
- Excess Charge — The difference between the Medicare-approved amount for a service or supply and the actual charge.
- Intermediaries — Organizations that process inpatient and outpatient claims on individuals by hospitals, skilled nursing facilities, home health agencies, hospices and certain other providers of health services.
- Limiting Charge — The maximum amount a physician may charge a Medicare beneficiary for a covered service if the physician does not accept assignment.
- Nonparticipating — Doctors or suppliers who may choose whether or not to accept assignment on each individual claim.
- Outpatient Physical and Occupational Therapy and Speech Pathology Services — Medically necessary outpatient physical and occupational therapy or speech pathology services prescribed by a doctor or therapist.
- Pap Smear Screening — Provides for a pap smear to screen for cervical cancer once every 2 years.
- Partial Hospitalization for Mental Health Treatment — A program of outpatient mental health care.
- Participating Doctor or Suppliers — Doctors and suppliers who sign agreements to become Medicare-participating. For example, they have agreed in advance to accept assignment on all Medicare claims.
- Peer Review Organizations — Groups of practicing doctors and other health care professionals who are paid by the government to review the care given to Medicare patients.
1. Part A Medicare Part A helps pay for inpatient hospital care, inpatient care in a skilled nursing facility, home health care, and hospice care.
An individual is eligible for Medicare Part A, Hospital Coverage, by qualifying for one of the following conditions:
- A citizen or a legal resident of the United States age 65 or over and qualified for Social Security or Railroad retirement benefits — Aged;
- Is 65 years old or over and entitled to monthly Social Security benefits based upon the spouse’s work record, and the spouse is at least 62;
- Is younger than 65 but has been entitled to Social Security disability benefits for 24 months — Disabled;
- Has End Stage Renal Disease (ESRD) — permanent kidney failure that requires dialysis or a transplant; and/or
- Has ALS (Amyotrophic Lateral Sclerosis, or Lou Gehrig’s disease) — automatically qualifies for Part A the month disability benefits begin.
Individuals who are not receiving those types of benefits need to sign up for Part A, even if they are eligible for premium-free Part A.
In addition, monthly Part A premiums are required when a beneficiary is not "fully insured" under Social Security, meaning they have not earned 40 quarters of coverage (the equivalent of 10 years of work), and therefore, are entitled to receive Social Security retirement, premium-free Medicare Part A, and survivor benefits. If the beneficiary has paid Medicare taxes for fewer than 30 quarters, the standard Part A premium is $506. If Medicare taxes have been paid for 30-39 quarters, the standard Part A premium is $278.
Those who want to sign up for Medicare Part A have the following three options:
- Initial enrollment period: when an individual first becomes eligible for Medicare (starting 3 months before turning age 65, ending 3 months after the 65th birthday);
- General enrollment period: between January 1 and March 31 each year;
- Special enrollment period: at any time during the year if the individual or his/her spouse is still employed and covered under a group health plan.
Those who are not eligible for premium-free Part A can purchase the coverage for a monthly premium. If individuals fail to sign up for Part A when they are first eligible, the monthly premium may go up 10% unless the person becomes eligible for a special enrollment period.
Inpatient Hospital Care — Hospital insurance helps pay for up to 90 days in a participating hospital in any benefit period, subject to a deductible. The first 60 days are covered at 100% of approved charges after the deductible is met. The next 30 covered days are paid, but they are paid with a daily copayment. Every Part A insured has a lifetime reserve of 60 days of hospital care. The lifetime reserve days have a copayment that is twice that of days 61 through 90, and they are nonrenewable. Covered services include semi-private room, meals, regular nursing services, operating and recovery room costs, hospital costs for anesthesia, intensive care, and coronary care, drugs, lab tests, X-rays, medical supplies, appliances, rehabilitation services, and preparatory services related to kidney transplant surgery. Blood is also covered, except for the first 3 pints.
Under the inpatient hospital stay, Part A does NOT include private duty nursing, a television, or telephone in your room. It also does not include a private room unless medically necessary. In addition, inpatient mental health care in a psychiatric facility is limited to 190 days in a lifetime.
Sixty (60) days of non-use of the inpatient hospital benefit starts a new benefit period and a new deductible.
Skilled Nursing Facility Care — Part A helps pay for up to 100 days in a participating skilled nursing facility in each benefit period, following a 3-day inpatient hospital stay for a related illness. To get this type of care, the insured's doctor must certify that daily skilled care is necessary. Covered expenses include semi-private room, meals, regular nursing and rehabilitation services, and other supplies.
Home Health Care — For an individual confined to the home and meeting certain other conditions, hospital insurance can pay the full approved cost of home health visits from a participating home health agency. There is no limit to the number of covered visits. Covered services include part-time skilled nursing care, physical therapy, and speech therapy. Hospital insurance also covers part-time services of home health aides, occupational therapy, medical social services, and medical supplies and equipment.
Hospice Care — Under certain conditions, hospital insurance can help pay for hospice care for terminally ill insureds if the care is provided by a Medicare-certified hospice. Covered services include doctor services, nursing services, medical appliances, supplies including outpatient drugs for pain relief, home health aide, homemaker services, therapies, medical social services, short-term inpatient care including respite care, and counseling.
Know This! Medicare Part A does not cover outpatient hospital care. That's covered under Medicare Part B.
Medicare Part A: Hospital Insurance Covered Service Reference Chart
BENEFIT MEDICARE PAYS YOU PAY HOSPITALIZATION: First 60 days All but the deductible Deductible Days 61-90 All but daily deductible Daily deductible After day 90 (up to 60 days)* All but daily deductible Daily deductible After lifetime reserve days Nothing All costs *60 lifetime reserve days. For each lifetime reserve day, Medicare pays all covered costs except for a daily coinsurance.
Part B Medicare Part B pays for doctor’s services and a variety of other medical services and supplies that are not covered by hospital insurance. Most of the services needed by people with permanent kidney failure are covered only by medical insurance.
Part B is optional and offered to everyone who enrolls in Part A. Part B is funded by monthly premiums and from the general revenues of the federal government. Most people enrolled in Medicare Part B pay the standard monthly premium. However, if an insured's modified adjusted gross income reported on IRS tax return is above a certain amount, the insured may be required to pay a higher premium.
When you become eligible for Part A, you are told that you will get and have to pay for Part B unless you decline it. If you later decide you want Part B after initially declining it, you must wait until the next general enrollment period (Jan. 1 through Mar. 31) to enroll.
After the annual medical insurance deductible is met, medical insurance will generally pay for 80% of the approved charges for covered expenses for the remainder of the year. There is no maximum out-of-pocket limit on the 20% coinsurance payable for Part B expenses.
Doctor Services — Part B covers doctor services no matter where received in the United States. Covered doctor services include surgical services, diagnostic tests and X-rays that are part of the treatment, medical supplies furnished in a doctor’s office, and services of the office nurse.
Outpatient Hospital Services — Part B covers outpatient hospital services received for diagnosis and treatment, such as care in an emergency room, outpatient clinic, or a hospital.
Home Health Visits — Medicare will pay for home health services as long as these services are recommended by the insured's doctor and the insured is eligible. However, these services are provided on a part-time basis with limits on the number of hours per day and days per week. The services that are not fully covered by Medicare will get coverage from Medicaid.
Other Medical and Health Services — Under certain conditions or limitations, medical insurance covers other medical services and supplies. Some examples are as follows: ambulance transportation; home dialysis equipment, supplies, periodic support services, independent laboratory tests, oral surgery, outpatient physical therapy, speech pathology services, and X-rays and radiation treatments.
Prescription Drugs (limited coverage) — Only medicines that are administered in a hospital outpatient department under certain circumstances, such as injected drugs at a doctor’s office, some oral cancer drugs, or drugs that require durable medical equipment (like a nebulizer or infusion pump), are covered. Other than the examples above, insured under Part B will have to pay 100% for most prescription drugs, unless covered by Part D.
Outpatient Treatment of Mental Illness — Medicare covers outpatient treatment of an approved condition (such as depression or anxiety) in a doctor's office or other health care provider's office or hospital outpatient department. Generally, the enrollee pays 20% of the Medicare-approved amount (coinsurance); Part B deductible also applies. Note that inpatient mental health care is covered under Part A.
Yearly "wellness" visit — In addition to a "Welcome to Medicare" preventive visit available during the first 12 months, Medicare Part B covers annual "wellness" visit during which the insured and the provider can develop or update a personalized plan for disease prevention. There is no out-of-pocket cost for the insured for these visits if the doctor or other qualified health care provider accepts assignments. If the doctor or the health care provider performs additional tests or services during the same visit that are not covered under this preventive benefit, the insured may have to pay coinsurance, and Part B deductible may also apply.
Medical insurance under Part B of Medicare does not cover the following:
- Private duty nursing;
- Skilled nursing home care costs over 100 days per benefit period;
- Intermediate nursing home care;
- Physician charges above Medicare’s approved amount;
- Most outpatient prescription drugs;
- Care received outside the United States;
- Custodial care received in the home;
- Dental care (except dental expenses resulting from an accident only), cosmetic surgery, eyeglasses, hearing aids, orthopedic shoes, acupuncture expenses; or
- Expenses incurred due to a war or act of war.
Medicare Part B: Medical Insurance Covered Services Reference Chart
BENEFIT MEDICARE PAYS YOU PAY MEDICAL EXPENSES: Medicare pays for medical services in or out of the hospital 80% of approved amount after the deductible Deductible*, plus 20% of approved amount and limited charges above approved amount CLINICAL LABORATORY SERVICES: Unlimited if medically necessary Generally 100% of approved amount Nothing for services HOME HEALTH CARE: For as long as you meet Medicare requirements for home health care benefits 100% of approved amount; 80% of approved amount for durable medical equipment Nothing for services; 20% of approved amount for durable medical equipment OUTPATIENT HOSPITAL TREATMENT: Unlimited if medically necessary Medicare payment to hospital based on hospital cost 20% of billed amount after the deductible BLOOD: Unlimited if medically necessary 80% of approved amount after the deductible, and starting with 4th pint First 3 pints plus 20% of approved amount for additional pints after the deductible** * Once you have reached a specified dollar amount in expenses for covered services, the Part B deductible does not apply to any other covered services you receive for the rest of the year.
** To the extent that any of the three pints of blood are paid for or replaced under one part of Medicare during the calendar year. They do not have to be paid for or replaced under the other part.
Part C The Medicare Modernization Act of 2003 changed the name of Part C from Medicare+Choice to Medicare Advantage. Medicare Advantage plans must cover all of the services covered under the Original Medicare except hospice care and some care in qualifying clinical research studies. However, Part C plans may have lower out-of-pocket costs than Original Medicare. They may also offer extra coverage, such as vision, hearing, dental, and other health and wellness programs.
To be eligible for Medicare Advantage, beneficiaries must also be enrolled in Medicare Parts A and B. Medicare Advantage is Medicare provided by an approved Health Maintenance Organization or Preferred Provider Organization. Many HMOs or PPOs do not charge premiums beyond what is paid by Medicare.
The advantages of an HMO or PPO for a Medicare recipient may be that there are no claims forms required, almost any medical problem is covered for a set fee so health care costs can be budgeted, and the HMO or PPO may pay for services not usually covered by Medicare or Medicare supplement policies, such as prescriptions, eye exams, hearing aids, or dental care.
Most Medicare HMOs require that medical services be received through the plan, except in emergencies. A few allow greater freedom of choice through point-of-service plans.
A Medicare Private Fee-for-Service Plan is a Medicare Advantage Plan offered by a private insurance company. Medicare pays a set amount of money every month to the private insurance company to provide health care coverage. The insurance company decides how much enrollees pay for the services they get.
Another section of Medicare Advantage Plan (Part C), Special Needs Plans, provides more focused and specialized health care for specific groups of people. This includes people who have both Medicare and Medicaid, who reside in a nursing home, or have certain chronic medical conditions.
Know This! Medicare Part C expands Original Medicare benefits through private health insurance programs.
Part D The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) was passed in November 2003. This act implemented a plan to add a Part D - Prescription Drug Benefit to the standard Medicare Coverages. This optional coverage is provided through private prescription drug plans (PDPs) that contract with Medicare. To receive the benefits provided, beneficiaries must sign up with a plan offering this coverage in their area and must be enrolled in Medicare Part A or in Parts A and B. In areas where no private plans are offered, the government will offer a standard plan. Medicaid recipients are automatically enrolled.
If Medicare beneficiaries don't enroll when they are first eligible, they must pay a 1% penalty for each month they delayed enrollment.
Medicare beneficiaries may choose between stand-alone plans that offer coverage on a fee-for-service basis, or integrated plans that group coverages together, including PPOs and HMOs (known as Medicare Advantage).
The plans offered by private companies are restricted by some standards set by Medicare, but still have freedom to personalize their plans. Providers must cover drugs for certain classes, but do not have to cover every drug in each class.
Those who sign up for the standard Prescription Drug Benefit plan will have a monthly premium and a deductible. The monthly premium varies by plan. After the deductible is paid, the plan would provide prescription drug costs coverage until a benefit limit is reached. Once the beneficiary and their plan spend $4,660 combined on drugs (including deductible), the beneficiary will generally pay no more than 25% of the cost for prescription drugs until their out-of-pocket spending is $7,400 (for 2023), under the standard drug benefit.
Once the beneficiary has reached their out-of-pocket spending, catastrophic coverage begins automatically. Catastrophic coverage will cover 95% of prescription drug costs. In most cases, the beneficiary will pay no more than 5% of the cost for covered drugs for the rest of the year.
Additional assistance will be available for those with low income. There will be no gap in coverage for these beneficiaries.
Know This! After the initial benefit limit is reached, a Prescription Drug Benefit plan will pay 75% of all generic and brand name drug costs.
Primary, Secondary Payor While an individual becomes eligible for Medicare upon turning age 65, federal laws extend primary coverage benefits under the employer’s plan to active older employees regardless of age. In other words, employer plans usually continue to be primary coverage, and Medicare is secondary coverage.
B. Medicare Supplement Policies
Medicare Supplement plans, referred to as Medigap, are policies issued by private insurance companies that are designed to fill in some of the gaps in Medicare. These plans are designed to fill the gap in coverage attributable to Medicare’s deductibles, copayment requirements, and benefit periods. These plans are not administered through the federal Social Security program, as is Medicare, but instead are sold and serviced by private insurers and HMOs. These policies must meet certain requirements and must be approved by the state department of insurance. Medicare Supplement policies pay some or all of Medicare’s deductibles and copayments.
Under the Omnibus Budget Reconciliation Act of 1990 (OBRA), Congress passed a law that authorized the NAIC to develop a standardized model for Medicare supplement policies. This model requires Medigap plans to meet certain requirements as to participant eligibility and the benefits provided. The purpose of this law was to eliminate questionable marketing practices and to provide consumers with a degree of protection and to standardize the protection afforded.
Know This! Medicare supplement plans are sold through private insurers, not federal health insurance programs.
Anyone who qualifies for Medicare may also purchase a Medicare Supplement and pay the necessary premium for those additional benefits. Under OBRA, Medicare supplement insurance may not discriminate in pricing or be denied on the basis of an applicant’s health status, claims experience, receipt of health care or medical condition. An open enrollment period is a 6-month period that guarantees the applicants the right to buy Medigap once they first sign up for Medicare Part B. In essence, to buy a Medigap policy, the applicant must generally have both Medicare Part A and Part B.
Medicare Supplement policies cannot be used to pay for Medicare Advantage (Part C) copayments, deductibles, or premiums. Additionally, insurers are prohibited from selling Medicare Supplement policies to anyone already enrolled in Medicaid.
In order to standardize the coverage provided under Medicare supplement policies, the NAIC has developed standard Medicare Supplement benefit plans which are identified with the letters A through N. The core benefits found in Plan A must be offered in all the plans, and the other plans have a variety of additional benefits. Plan A must be offered by any insurer marketing Medigap plans, while the other plans are optional.
Once a person becomes eligible for Medicare supplement plans, and during the open enrollment period, coverage is offered on a guaranteed issue basis. In these situations, an insurance company must do the following:
- Sell the patient a Medicare supplement policy;
- Cover all pre-existing conditions incurred more than 6 months from the effective date of coverage; and
- Not charge more for a supplement policy because of past or present health problems.
Medicare Supplement Plan A provides only the core benefits. The core benefits, also known as basic benefits, cover the following:
- Part A coinsurance/copayment (NOT Part A deductible);
- Part A hospital costs up to an additional 365 days after Medicare benefits are used up;
- Part A hospice care coinsurance/copayment;
- Part B coinsurance/copayment; and
- The first 3 pints of blood ("blood deductible" for Parts A and B).
In addition to Plan A, which offers only the core benefits, most insurers also offer some or all of the additional plans. Insurers are not allowed to change the benefits offered in these supplemental plans, nor may they change the designation letter of any of the plans.
- Plan B – Core benefits plus Medicare Part A deductible.
- Plan D – Core benefits, Medicare Part A deductible, skilled nursing facility coinsurance, and the foreign travel benefit.
- Plan G – Core benefits, Medicare Part A deductible, skilled nursing facility coinsurance, 100% of Medicare Part B excess charges, and the foreign travel benefit. This plan must pay for services of activities of daily living (ADL) that Medicare doesn't cover.
- Plans C, E, F, H, I and J are no longer available. These plans will remain in force for those insureds who purchased them when they were still available.
- Medicare Supplement Plans K and L are lower premium plans with higher out-of-pocket costs. The core benefits are different in these 2 plans as well:
Plan K:
- Approved hospital costs for the copayments for days 61 through 90 in any Medicare benefit period.
- Approved hospital costs for the copayments for lifetime reserve days 91 through 150.
- Approved hospital costs for an additional 365 days after all Medicare benefits are used up.
- 50% of charges for the first 3 pints of blood.
- 50% of Part B coinsurance amount.
- 50% of hospice cost-sharing and respite care expenses for Part A.
- Includes 50% of the Medicare Part A deductible and 50% of skilled nursing facility coinsurance.
Plan L:
- Approved hospital costs for the copayments for days 61 through 90 in any Medicare benefit period.
- Approved hospital costs for the copayments for lifetime reserve days 91 through 150.
- Approved hospital costs for an additional 365 days after all Medicare benefits are used up.
- 75% of charges for the first 3 pints of blood.
- 75% of Part B coinsurance amount.
- 75% of hospice cost-sharing and respite care expenses for Part A.
- Includes 75% of the Medicare Part A deductible and 75% of skilled nursing facility coinsurance.
Plans M and N provide benefits similar to Plan D, but the co-pays and deductibles might be different.
This table outlines the benefits provided under each of the Medigap plans available.
Know This! All Medicare supplement plans must offer the core benefits available in Plan A.
Other Requirements — Insurers are required to use the same format, language, and definitions in describing the benefits available in each of the Medigap plans. They are required to use a standardized chart and outline that summarizes the benefits.
Although insurers are not allowed to alter the standardized benefits offered in each of these plans, they are allowed to offer new, innovative benefits which can be proven cost-effective and which are not currently available in the marketplace. All Medigap policies are guaranteed renewable. The insurance company cannot cancel or nonrenew coverage except for nonpayment of the premium or because of material misrepresentation on the application. In addition, although the benefits provided by these plans are identical from one company to the next, the premiums vary greatly. Depending on how the insurer determines the premium charge, they can usually increase premiums on the policy anniversary date.
Medigap policies must also include a 30-day free-look provision that allows the insured to return the policy to the insurer within 30 days for a full refund of the premium paid.
Medigap policies cannot include a provision that restricts coverage for pre-existing conditions for more than 6 months. In addition, if the insured has had a Medigap policy for at least 6 months and decides to change to another policy, the new policy cannot have a waiting period for pre-existing conditions for the same coverage that was included in the old policy. If the replacement policy includes additional coverage that was not in the old policy, then the 6-month waiting period can be applied, but only as it pertains to the additional coverages.
A Medicare SELECT policy is a Medicare supplement policy that contains restricted network provisions — provisions that condition the payment of benefits, in whole or in part, on the use of network providers. SELECT plans negotiate with a provider network of doctors, hospitals and specialists to charge lower rates for medical services. It essentially operates like an HMO. These lower rates keep costs down for the SELECT plan provider, and plan members pay lower premiums.
Each Medicare SELECT policy must be approved by the head of a state's department of insurance. Currently, issuers are not allowed to sell new Medicare SELECT policies to individuals whose primary residence is located outside of the issuer’s service area.
Every Medicare SELECT policy must do the following:
- Provide payment for full coverage under the policy for covered services not available through network providers;
- Not restrict payment for covered services provided by non-network providers if the services are for symptoms requiring emergency care and it is not reasonable to obtain such services through a network provider;
- Make full and fair disclosure in writing of the provisions, restrictions, and limitations of the Medicare SELECT policy to each applicant;
- Make available upon request the opportunity to purchase a Medicare supplement policy offered by the issuer which has comparable benefits and does not contain a restricted network provision. These policies must be available without requiring evidence of insurability if the Medicare SELECT policy has been in force for 6 months; and
- Provide for continuation of coverage in the event that Medicare SELECT policies are discontinued due to the failure of the Medicare SELECT program.
C. Medicaid
Medicaid is a federal- and state-funded program for those whose income and resources are insufficient to meet the cost of necessary medical care. Individual states design and administer the Medicaid programs (typically through the state's Department of Public Welfare) under broad guidelines established by the federal government.
To qualify for Medicaid, individuals must meet income and other eligibility requirements. Once a person is determined to qualify with low income and low assets, the person must meet other qualifiers, some of which are blindness, disability, pregnancy, age (over 65), or caring for children receiving welfare benefits. For many eligibility groups, income is calculated in relation to a percentage of the Federal Poverty Level (FPL).
After the implementation of the Affordable Care Act, new, modernized rules regarding verification of Medicaid eligibility will mean that state Medicaid agencies will rely primarily on information available through data sources (such as the Social Security Administration, the Departments of Homeland Security and Labor) rather than paper documentation from families. Each state has prepared a verification plan for Medicaid in order to comply with the new rules.
In addition to certain levels of income and assets, there are other nonfinancial eligibility criteria that are used in determining Medicaid eligibility. In order to be eligible for Medicaid, individuals need to satisfy federal and state requirements regarding residency, immigration status, and documentation of U.S. citizenship.
Medicaid mandates that the states provide at least the following services:
- Physician’s services;
- Inpatient hospital care;
- Outpatient hospital care;
- Skilled nursing home services;
- Laboratory and x-ray services;
- Home health care services;
- Rural health clinic services;
- Periodic screening, diagnosis, and treatment;
- Family planning services; and
- Medicaid also pays for prescription drugs, dental services, private duty nursing services, eyeglasses, check-ups, and medical supplies and equipment.
D. Long-Term Care Policies
Long-term care policies, which can be marketed in the form of individual policies, group policies, or as riders to life insurance policies, provide coverage for individuals who are no longer able to live an independent lifestyle and require living assistance at home or in a nursing home facility. Long-term care policies can vary in the number of days of confinement covered, the number of home health visits covered, the amount paid for nursing home care, and other contract provisions. They also must provide coverage for at least 12 consecutive months in a setting other than an acute care unit of a hospital.
Long-term care policies usually include an elimination (waiting) period similar to those found in disability income policies. Long-term care elimination periods may range from 0 to 365 days (make sure to check your state-specific requirement in the regulations section). The longer the waiting period, the lower the premium. Insurers usually give insureds an option to select the elimination period that best suits their needs. LTC policies also define the benefit period for how long coverage applies, after the elimination period. The benefit period is usually 2 to 5 years, with a few policies offering lifetime coverage. The longer the benefit period, the higher the premium will be.
The benefit amount payable under most LTC policies is usually a specific fixed dollar amount per day, regardless of the actual cost of care. For example, if an insured has a fixed daily coverage of $100 and the care facility only charges $90 a day, the insurance company will pay the full amount of $100 a day. Some policies pay the actual charge incurred per day. Most LTC policies are also guaranteed renewable; however, insurers do have the right to increase the premiums.
Know This! LTC policies must be guaranteed renewable.
For an additional premium, optional benefits are available with long-term care policies.
The following are prohibited provisions or actions in long-term care policies:
- Cancel, nonrenew, or otherwise terminate a LTC policy on the grounds of the insured's age or the deterioration of mental or physical condition.
- Establish a new waiting period when coverage is converted or replaced within the same company, except for increased benefits voluntarily selected by the insured.
- Cover only skilled nursing care or provide significantly more coverage for skilled care than lower levels of care.
Long-term care policies may have the following exclusions:
- Pre-existing conditions or diseases.
- Mental and nervous disorders or disease (except for organic cognitive disorders such as Alzheimer's disease, senile dementia, and Parkinson's disease).
- Alcoholism and drug addiction.
- Treatment or illness caused by war, participation in criminal activities, or attempted suicide.
- Treatment payable by the government, Medicare, workers compensation, or similar coverage.
1. Eligibility for Benefits
Normally to be eligible for benefits from a long-term care policy, the insured must be unable to perform some of the activities of daily living (ADLs). Activities of daily living include bathing, dressing, toileting, transferring positions (also called mobility), continence, and eating.
2. Levels of Care
Generally, long-term care policies will cover 3 levels of care: skilled nursing care, intermediate care, and custodial care. In addition to these levels of care, the long-term care policy may provide coverage for home health care, adult day care, hospice care, or respite care, all of which can be received at home.
-
Skilled care is daily nursing and rehabilitative care that can only be provided by medical personnel, under the direction of a physician. Skilled care is almost always provided in an institutional setting. Examples of skilled care include changing sterile dressing and physical therapy given in a skilled nursing care facility. Care that can be given by nonprofessional staff is not considered skilled care.
-
Intermediate care is occasional nursing or rehabilitative care provided for stable conditions that require daily medical assistance on a less frequent basis than skilled nursing care. It is ordered by a physician, and skilled medical personnel would deliver or monitor this type of care. Intermediate care could be as simple as giving medication to a group in physical therapy once a day or changing a bandage. It may be carried out in a nursing home, an intermediate-care unit, or in the patient’s home.
-
Custodial care is care for meeting personal needs such as assistance in eating, dressing, or bathing, which can be provided by nonmedical personnel, such as relatives or home health care workers. Custodial care can be provided in an institutional setting or in the patient’s home. In other words, it involves caring for a person's activities of daily living, and not hospital or surgical needs.
Know This! Skilled care and intermediate care require the assistance of medically licensed personnel. Custodial care may be administered by nonmedical personnel.
-
Home health care is care provided by a skilled nursing or other professional services in one’s home. Home health care includes occasional visits to the person’s home by registered nurses, licensed practical nurses, licensed vocational nurses, or community-based organizations like hospice. Home health care might include physical therapy, occupational therapy, speech therapy, and medical services by a social worker.
-
Home Convalescent Care is provided in the insured’s home under a planned program established by the insured's attending physician. Such care must be provided by a long-term care facility, a home health care agency, or a hospital.
-
Residential Care is provided while the insured resides in a retirement community or a residential care facility for the elderly (RCFE). In some arrangements, the degree of independence is the same as living in one's own home; however, this care provides a physical and social environment that contributes to continued intellectual, psychological, and physical growth. These facilities are commonly for the middle and upper classes because of the costs.
-
Adult day care is care provided for functionally impaired adults on less than a 24-hour basis. It could be provided by a neighborhood recreation center or a community center. Care includes transportation to and from the day care center, and a variety of health, social, and related activities. Meals are usually included as a part of the service.
-
Respite Care is designed to provide relief to the family caregiver and can include a service such as someone coming to the home while the caregiver takes a nap or goes out for a while. Adult day care centers also provide this type of relief for the caregiver.
3. Individual LTC Contracts
Individual long-term care insurance is the most common LTC in the private market. The advantages to an individual long-term care policy include state regulation of LTC plans, guaranteed renewability, and the ability to customize the plan to the individual's own needs.
4. Group and Voluntary LTC Contracts
Group long-term care policies are gaining in popularity. Like other group health insurance, group LTC offers lower rates and less underwriting, allowing someone who might be denied individual coverage to enroll in open enrollment periods. Not all states regulate group LTC, and many group plans do not offer employer contributions to premiums. Most group LTC plans are voluntary, meaning the individual decides whether or not to enroll in the plan.
E. Chapter Recap
This chapter explained health insurance available to senior citizens and special needs individuals: Medicare, Medicare Supplements, Medicaid, and Long-term Care. Let's recap some of the key points:
MEDICARE
Basics
- Federal medical expense insurance program for people who:
- Are age 65 or older
- Have been entitled to Social Security disability income benefits for 2 years
- Have permanent kidney failure (ESRD)
- 4 parts:
- Part A, Hospital Insurance, financed through payroll tax (FICA)
- Part B, Medical Insurance, financed by insureds and general revenues
- Part C, Medicare Advantage, allows for receipt of health care services through available provider organizations
- Part D, Prescription Drug coverage
Part A
- Enrollment:
- Initial enrollment period - when an individual first becomes eligible for Medicare (starting 3 months before turning age 65, ending 3 months after the 65th birthday)
- General enrollment period - between January 1st and March 31st each year
- Special enrollment period - at any time during the year if the individual or his/her spouse is still employed and covered under a group health plan
- Coverage:
- Inpatient Hospital Care
- Skilled Nursing Facility Care
- Home Health Care
- Hospice Care
Part B
- Optional; offered to everyone who enrolls in Part A
- Coverage:
- Doctor Services
- Outpatient Hospital Services
- Home Health Visits
- Other Medical and Health Services
- Prescription Drugs (limited coverage)
- Outpatient Treatment of Mental Illness
- Yearly wellness visit
Part C
- Medicare Advantage: requires enrollment in Parts A and B
- Provided by an approved Health Maintenance Organization or Preferred Provider Organization
Part D
- Prescription drug benefit
- Optional coverage through private prescription plans that contract with Medicare
Primary, Secondary Payor
- For individuals eligible for Medicare coverage who continue to work, the employer’s health plan would be primary coverage while Medicare would be secondary coverage
MEDICARE SUPPLEMENT POLICIES
Basics
- Referred to as Medigap
- Policies issued by private insurance companies to fill in gaps in Medicare
- Open enrollment period of 6-months
Coverage
- Plan A: core benefits, such as coinsurance/copayment; additional Part A hospital costs; hospice care coinsurance / copayment; Part B coinsurance/copayment; 3 pints of blood under Parts A and B
- Plans B – N: core benefits + various additional benefits
MEDICAID
- Medicaid Medical care for those whose income and resources are insufficient
- Federal and state funded
LONG-TERM CARE POLICIES
Policies
- Available as individual policies, group policies, or as riders to life insurance policies
- Coverage for individuals who require living assistance at home or in a nursing home facility
- Must provide at least 12 months of consecutive coverage in a setting other than an acute care unit of a hospital
- Guaranteed renewable, but insurers may increase premiums
Levels of Care
Skilled care - daily nursing and rehabilitative care provided by medical personnel Intermediate care - occasional nursing or rehabilitative care provided for stable conditions that require daily medical assistance on a less frequent basis than skilled nursing care Custodial care - care for meeting personal needs such as assistance in eating, dressing, or bathing, which can be provided by nonmedical personnel, such as relatives or home health care workers Home health care is care provided by a skilled nursing or other professional services in one’s home. Home Convalescent Care is provided in the insured’s home under a planned program established by the insured's attending physician. Residential Care is provided while the insured resides in a retirement community or a residential care facility for the elderly (RCFE). Adult day care is care provided for functionally impaired adults on less than a 24-hour basis. Respite Care is designed to provide relief to the family caregiver, and can include a service such as someone coming to the home while the caregiver takes a nap or goes out for a while.
Individual LTC Contracts
- Individual long-term care insurance is the most common LTC in the private market.
- Advantages include state regulation of LTC plans, guaranteed renewability, and the ability to customize the plan to the individual's own needs.
Group and Voluntary LTC Contracts
- Group long-term care policies are gaining in popularity.
- Like other group health insurance, group LTC offers lower rates and less underwriting.
- Not all states regulate group LTC, and many group plans do not offer employer contributions to premiums.
- Most group LTC plans are voluntary, meaning the individual decides whether or not to enroll in the plan.
-
Federal Tax Considerations for Accident and Health Insurance
Federal Tax Considerations for Accident and Health InsuranceFederal Tax Considerations For Accident And Health Insurance
Different types of health insurance policies are subject to a different degree of taxation. This section will continue the discussion of tax issues as they pertain to health insurance, specifically the tax treatment of premiums and proceeds. By the end of this section, you should be able to compare the taxation of personally-owned health insurance policies with similar policies provided by an employer. You will also learn about business disability insurance and reimbursement or savings accounts available in group coverage.
TERMS TO KNOW
- Adjusted gross income — gross income (all income from whatever sources) minus adjustments to income
- Defined-benefit plans — the employer specifies an amount of benefits promised to the employee
- Defined-contribution plans — focus on contributions rather than on the benefits they will pay out
- IRS — Internal Revenue Service: a U.S. Government agency responsible for collecting of taxes, and enforcement of the Internal Revenue Code
- Tax deductible — a qualified expense that may reduce the amount of income subject to taxation
- Tax exempt — not subject to taxation
- Taxable — subject to taxation
A. Individual Health Insurance
Taxation of insurance benefits is often determined by whether or not the premiums were taxed. Premium payments on personally owned disability income policies are nondeductible by the individual. However, disability income benefits are received income tax-free by the individual. In medical expense insurance policies, unreimbursed medical expenses paid for the insured, the insured's spouse, and dependents may be claimed as deductions if the expenses exceed a certain percentage of the insured's adjusted gross income. The law permits deductions for unreimbursed expenses in excess of 7.5% of the adjusted gross income (AGI). This provision only applies if the insured itemizes these deductions on his/her tax return.
Long-term care premium payments are deductible as a medical expense to the extent that when added to all other unreimbursed medical expenses, the total exceeds 10% of the taxpayer’s adjusted gross income if the taxpayer itemizes his/her deductions. However, there is a limit on the amount of premium that can be deducted depending on the age of the insured (taxpayer) at the end of the year. The IRS sets annual limits for that amount, and any premium above these limits will not be considered a medical expense, and therefore, cannot be tax deductible.
B. Group Disability Income
Premiums paid by the employer for disability income insurance for its employees are deductible as a business expense and are not considered taxable income to the employee. Benefits received by an employee that are attributable to employer contributions are fully taxable to the employee as income. When the employer and employee share in disability insurance premium contributions, the employee’s contribution is not deductible; however, benefits received by the employee that are attributable to the employee's portion of the contribution are not taxable as income. The taxation of income received by the employee would depend on the type of a group plan:
- Noncontributory – The employer pays the entire cost of the disability insurance premium, so the income benefits are included in the employee’s gross income and taxed as ordinary income.
- Fully contributory – The employee pays the entire cost of the disability insurance premium, so the income benefits are received income tax-free by the employee.
- Partially contributory – The cost of disability insurance is paid partially by the employer and partially by the employee. The portion paid by the employee is received income tax-free, and the portion paid by the employer is included in the employee’s gross income and taxed as ordinary income.
For example, if an employee contributes 40% of the premium and receives a benefit of $1,000, only $600 (60% = employer contribution) of the benefit payment will be taxed to the employee as income, while $400 (40% = employee contribution) will be received tax-free.
Know This! Disability insurance premiums are deductible as a business expense; benefits are taxable income for employee.
Short-term disability (STD) group plans usually have a benefit period of less than 2 years. It is common in this type of disability income plans to place a maximum dollar amount on the benefit that will be provided regardless of earnings, and to have an elimination period (except for disability resulting from accidents). Long-term disability (LTD) group plans usually pay benefits for 2 years or longer.
1. Benefits Subject to FICA
Benefits paid to disabled employees that are attributable to the employer’s contribution are subject to Federal Insurance Contributions Act (FICA) withholding for Social Security purposes. Any portion of the benefit paid for and deducted by the employer will be considered taxable income to the employee.
C. Business Disability Insurance
1. Key Person Disability Income
Key person disability income premiums are not deductible to the business, but the benefits are received income tax-free by the business.
2. Disability Buy-Sell
Disability buy-sell insurance is typically written to cover partners or corporate officers of a closely held business. The policy provides funds for the business organization to purchase the business interest of a disabled partner. In a disability buy-sell policy, whether a cross-purchase or entity, the premiums are not deductible to the business, but the benefits are received income tax-free by the business.
3. Business Overhead Expense
Business overhead expense (BOE) insurance is sold to small business owners to reimburse them for the overhead expenses after a disability. The premiums paid to the BOE policy are tax deductible to the business as a business expense. The benefits are usually limited to covered expenses incurred or the maximum monthly benefit stated in the policy and are taxable to the business as received.
D. Consumer Driven Health Plans
1. Health Savings Account (HSAs)
Health savings accounts (HSAs) are designed to help individuals save for qualified health expenses that they, their spouse, or their dependents incur. An individual who is covered by a high deductible health plan can make a tax-deductible contribution to an HSA and use it to pay for out-of-pocket medical expenses. Contributions by an employer are not included in the individual's taxable income. Health Savings Accounts (HSAs) feature tax-deferred growth, and enable the insured to pay for medical expenses with pre-tax income. Excess funds can be carried over to the next year. Regardless of how income is earned, any money deposited into an HSA is considered an "above-the-line" deduction, giving a 100% write-off against adjusted gross income. Health Savings Accounts provide a broad range of tax-free withdrawals including for the following benefits and services:
- Doctors, dentists and hospitals;
- Artificial limbs;
- Drugs;
- Eyeglasses and contacts;
- Chiropractic;
- Laboratory expenses;
- Nursing home costs;
- Physical therapy;
- Psychoanalysis;
- X-rays; and
- Nursing home insurance premiums.
2. Health Reimbursement Account (HRAs)
Health Reimbursement Accounts (HRAs) consist of funds set aside by employers to reimburse employees for qualified medical expenses, such as deductibles or coinsurance amounts. Employers qualify for preferential tax treatment of funds placed in an HRA in the same way that they qualify for tax advantages by funding an insurance plan. Employers can deduct the cost of a health reimbursement account as a business expense. The following are key characteristics of HRAs:
- They are contribution healthcare plans, not defined benefit plans;
- Not a taxable employee benefit;
- Employers' contributions are tax deductible;
- Employees can roll over unused balances at the end of the year;
- Employers do not need to advance claims payments to employees or healthcare providers during the early months of the plan year;
- Provided with employer dollars, not employee salary reductions;
- Permit the employer to reduce health plan costs by coupling the HRA with a high-deductible (and usually lower-cost) health plan; and
- Balance the group purchasing power of larger employers and smaller employers.
In Health Reimbursement Accounts (HRAs), the employer's contribution is tax deductible in the year in which the reimbursement is made to the employee. The employee is not taxed on receipt of the benefit. Benefits must be paid solely to the employee for medical care expenses for the employee, the employee's spouse, or dependents. If funds are distributed for other than medical care expenses, the benefit is considered to be taxable income to the employee.
3. Flexible Spending Accounts (FSAs)
A Flexible Spending Account (FSA) is a form of cafeteria plan benefit funded by salary reduction and employer contributions. The employees are allowed to deposit a certain amount of their paycheck into an account before paying income taxes. Then, during the year, the employee can be directly reimbursed from this account for eligible health care and dependent care expenses. FSA benefits are subject to an annual maximum and "use-or-lose" rule. This plan does not provide a cumulative benefit beyond the plan year.
There are 2 types of Flexible Spending Accounts: a Health Care Account for out-of-pocket health care expenses and a Dependent Care Account (subject to annual contribution limits) to help pay for dependent's care expenses, which makes it possible for an employee and their spouse to continue to work. An FSA is exempt from federal income taxes, Social Security (FICA) taxes, and, in most cases, state income taxes, saving 1/3 or more in taxes. If the plan favors highly compensated employees, the benefits for the highly compensated employees are not exempt from federal income taxes.
Know This! FSAs may be used to pay medical and dental expenses for employees and their dependents. Child and dependent care expenses must be for the care of one or more qualifying persons:
- A dependent who was under age 13 when the care was provided and who can be claimed as an exemption on the employee's Federal Income Tax return;
- A spouse who was physically or mentally not able to care for himself or herself; or
- A dependent who was physically or mentally not able to care for himself or herself and who can be claimed as an exemption (as long as the person is earning gross income less than an IRS-specified amount).
Persons who cannot dress, clean, or feed themselves because of physical or mental problems are considered not able to care for themselves. Also, persons who must have constant attention to prevent them from injuring themselves or others are considered not able to care for themselves. The insured may change benefits during open enrollment. After that period, generally, no other changes can be made during the plan year. However, the insured might be able to make a change under one of the following circumstances, referred to as qualified life event changes:
- Marital status;
- Number of dependents;
- One of dependents becomes eligible for or no longer satisfies the coverage requirements under the Medical Reimbursement plan for unmarried dependents due to attained age, student status, or any similar circumstances;
- The insured, the insured's spouse's or qualified dependent's employment status that affects eligibility under the plan (at least a 31-day break in employment status to qualify as a change in status);
- Change in dependent care provider; or
- Family medical leave.
The IRS limits the annual contribution for Dependent Care Accounts to a specified amount that gets adjusted annually for the cost of living. This is a family limit, meaning that even if both parents have access to flexible care accounts, their combined contributions cannot exceed the amount.
4. High Deductible Health Plans (HDHPs)
High-deductible health plans (HDHPs) are often used in coordination with Medical Savings Accounts (MSAs), Health Savings Accounts (HSAs), or Health Reimbursement Accounts (HRAs). The high-deductible health plan features higher annual deductibles and out-of-pocket limits than traditional health plans, which means lower premiums. Except for preventive care, the annual deductible must be met before the plan will pay benefits. Preventive care services are usually first-dollar coverage or paid after copayment. The HDHP credits a portion of the health plan premium into the coordinating MSA, HSA, or HRA on a monthly basis. The deductible of the HDHP may be paid with funds from the coordinating account plan.
High-deductible health plans (HDHPs) are taxed in the same manner as other traditional health plans.
Tax Considerations for Health Insurance
PREMIUMS BENEFITS Individual Disability Income Not deductible Group Disability Income Deductible for employer Individual Medical Not deductible* Group Medical Deductible for employer Individual Long-Term Care Not deductible* Group Long-Term Care Deductible for employer Individual Medicare Supplement Not deductible* Group Medicare Supplement Deductible for employer Buy-Sell Not deductible Key Person Not deductible Business Overhead Expense (BOE) Deductible for employer MSAs Deductible FSAs Not deductible HRAs Deductible HSAs Deductible - Unless combined premiums and unreimbursed medical expenses exceed 10% of adjusted gross income (or 7.5% for individuals age 65 or older), and subject to the tax-qualified limitations. Please note that not all plans are discussed in every state. Refer to your text to learn which plans apply in your state.
E. Chapter Recap
This chapter explained taxation of various health insurance policies. Let's recap some of the major points:
TAX TREATMENT OF PREMIUMS AND PROCEEDS
Personally-Owned Health Insurance
- Premium payments nondeductible
- Benefits received tax-free
Employer-Provided Health Insurance
- Premium payments made by employer deductible as a business expense
- Benefits received by employee taxable to employee as income
Types of employer health plans:
- Noncontributory - employer pays entire cost; benefits part of employee's gross income and taxed income
- Fully contributory - employee pays entire cost; benefits received tax-free by employee
- Partially contributory - cost shared by employer and employee; portion paid by employee is received tax-free, and portion paid by employer is part of employee's gross income and taxed as ordinary income
Medical and dental expense - employer premiums are deductible; premium by the employee is not deductible
Long-term care - premiums are deductible; daily benefits that do not exceed costs are tax-free; excess costs are taxed
Accidental death and dismemberment - policies are deductible to the employer; benefits are tax-free
Business Disability
Key Person:
- Premium not tax deductible to business
- Benefits tax-free by business
Buy-sell agreement:
- Premiums not deductible to business
- Benefits tax-free by business
Business Overhead Expense (BOE):
- Deductible for employer
- Taxable
Consumer-driven Plans
HSAs - tax-deferred growth; excess funds can be carried over to the next year
HRAs - contribution plans; employee's contribution tax deductible
FSAs - salary reduction and employer contribution; annual maximum and use-or-lose rule
Know This! FSAs may be used to pay medical and dental expenses for employees and their dependents.
Child and dependent care expenses must be for the care of one or more qualifying persons:
- A dependent who was under age 13 when the care was provided and who can be claimed as an exemption on the employee's Federal Income Tax return;
- A spouse who was physically or mentally not able to care for himself or herself; or
- A dependent who was physically or mentally not able to care for himself or herself and who can be claimed as an exemption (as long as the person is earning gross income less than an IRS-specified amount).
Persons who cannot dress, clean, or feed themselves because of physical or mental problems are considered not able to care for themselves. Also, persons who must have constant attention to prevent them from injuring themselves or others are considered not able to care for themselves. The insured may change benefits during open enrollment. After that period, generally, no other changes can be made during the plan year. However, the insured might be able to make a change under one of the following circumstances, referred to as qualified life event changes:
- Marital status;
- Number of dependents;
- One of dependents becomes eligible for or no longer satisfies the coverage requirements under the Medical Reimbursement plan for unmarried dependents due to attained age, student status, or any similar circumstances;
- The insured, the insured's spouse's or qualified dependent's employment status that affects eligibility under the plan (at least a 31-day break in employment status to qualify as a change in status);
- Change in dependent care provider; or
- Family medical leave.
The IRS limits the annual contribution for Dependent Care Accounts to a specified amount that gets adjusted annually for the cost of living. This is a family limit, meaning that even if both parents have access to flexible care accounts, their combined contributions cannot exceed the amount.
High Deductible Health Plans (HDHPs)
High-deductible health plans (HDHPs) are often used in coordination with Medical Savings Accounts (MSAs), Health Savings Accounts (HSAs), or Health Reimbursement Accounts (HRAs). The high-deductible health plan features higher annual deductibles and out-of-pocket limits than traditional health plans, which means lower premiums. Except for preventive care, the annual deductible must be met before the plan will pay benefits. Preventive care services are usually first-dollar coverage or paid after copayment. The HDHP credits a portion of the health plan premium into the coordinating MSA, HSA, or HRA on a monthly basis. The deductible of the HDHP may be paid with funds from the coordinating account plan. High-deductible health plans (HDHPs) are taxed in the same manner as other traditional health plans.
Tax Considerations for Health Insurance
-
Arkansas Statutes, Rules & Regulations for Life & Health
Arkansas Statutes, Rules & Regulations for Life & Health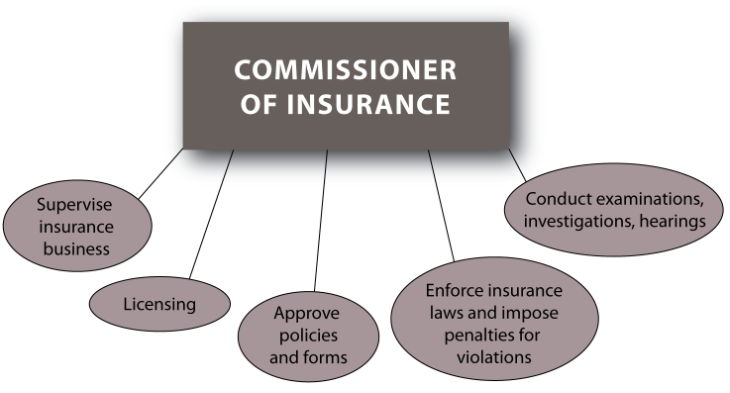
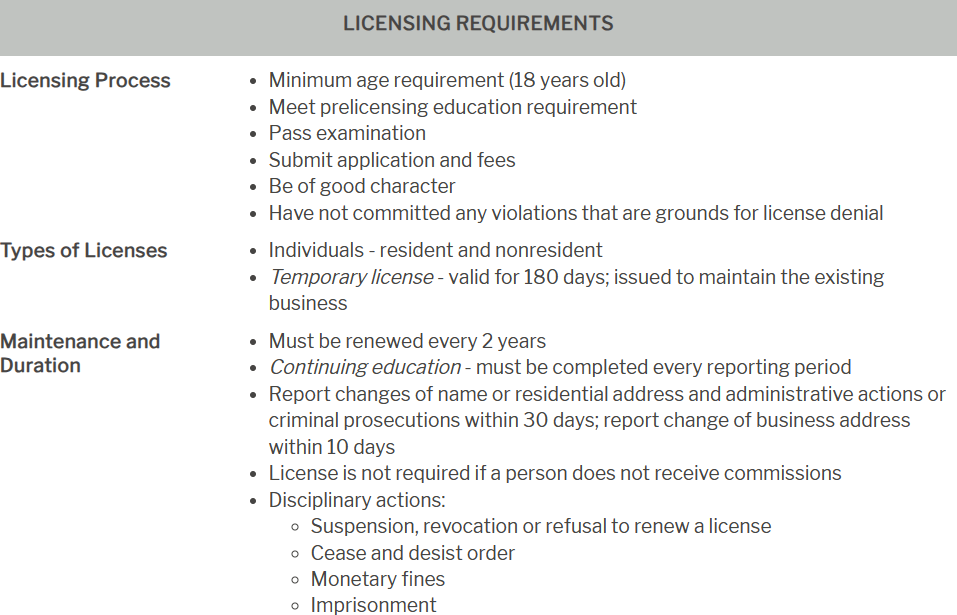
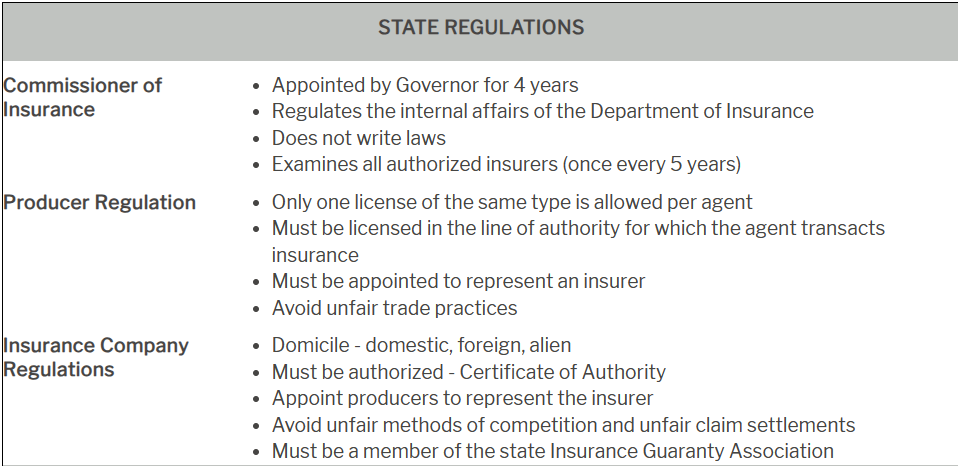
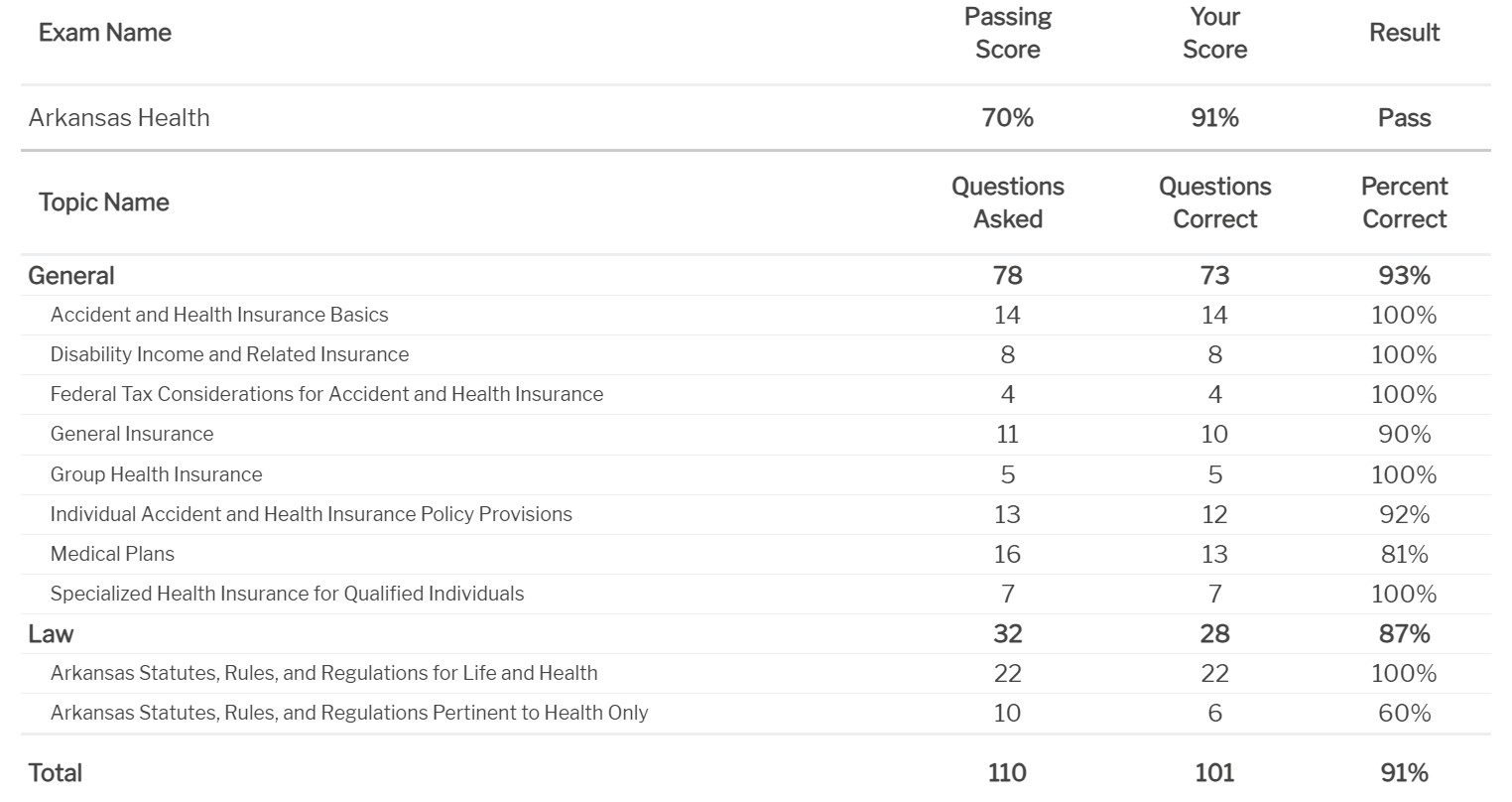
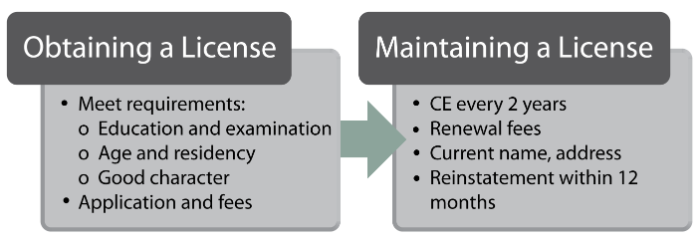
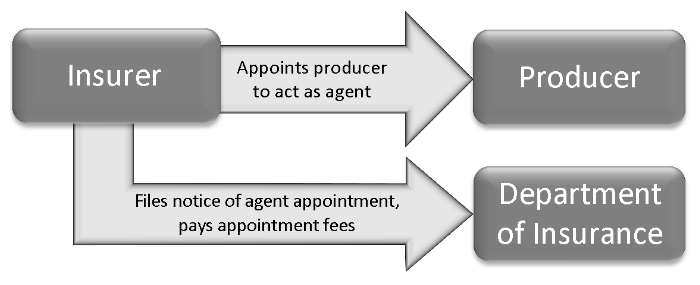
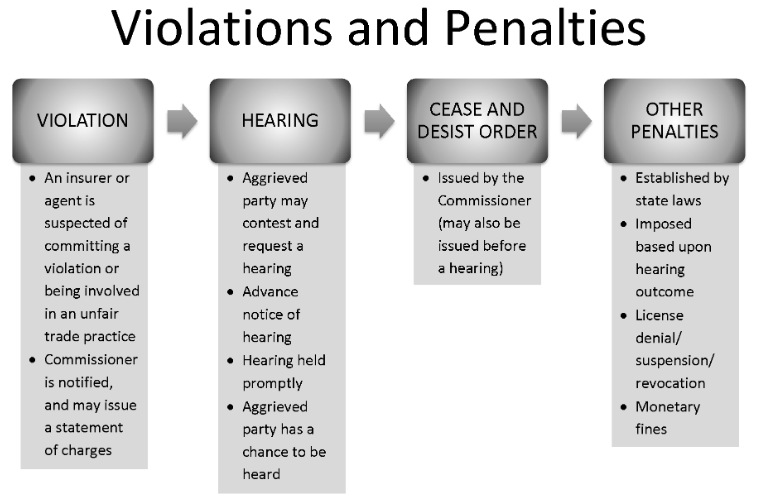
Arkansas Statutes, Rules, And Regulations For Life And Health
This chapter explains some of the important state regulations that apply to life and health insurance policies. As you are reading about different types of policies, pay close attention to the specific rules and requirements for insurers and producers, as well as policy standards outlined in the Insurance Code of this state.
TERMS TO KNOW
- Cease and desist — to stop or discontinue
- Coercion — forceful act or threat aimed to influence a person to act against his or her will
- Commission — payment to the agent by the insurance company for placing insurance, usually a percentage of the policy premium
- Commissioner — the head of the State Department of Insurance
- Exempt — not subject to an obligation
- Home office — insurer's headquarters, principal place of business
- Inducement — an offer that attempts to influence the other party
- Solvency — ability to meet financial obligations (e.g. an insurance company maintains enough assets to pay claims)
- Statute — a formal written law enacted by legislature; insurance statutes can be found in the state Insurance Code
A. Insurance And Insurers - General Definitions
1. Insurance Transaction The term insurance transaction includes any of the following (by mail or any other means):
- Solicitation;
- Negotiations;
- Sale (effectuation of a contract of insurance); and
- Advising an individual concerning coverage or claims.
2. Domestic, Foreign, and Alien Companies Insurance companies are classified according to the location of incorporation (domicile). Regardless of where an insurance company is incorporated, it must obtain a Certificate of Authority before transacting insurance within the state.
Know This! A domicile refers to the location where an insurer is incorporated, not necessarily where the insurer conducts business.
-
A domestic insurer is an insurance company that is incorporated in this state. In most cases, the company's home office is in the state in which it was formed—the company's domicile. For instance, a company chartered in Pennsylvania would be considered a Pennsylvania domestic company.
-
A foreign insurer is an insurance company that is incorporated in another state, the District of Columbia, or a territorial possession. Currently, the United States has 5 major U.S. territories: American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, and the U.S. Virgin Islands. For example, a company chartered in California would be a foreign insurer within the state of New York. A company chartered in Puerto Rico will be foreign in any U.S. state.
-
An alien insurer is an insurance company that is incorporated outside the United States.
3. Stock and Mutual Companies The following are the most common types of ownership.
-
Stock companies are owned by the stockholders who provide the capital necessary to establish and operate the insurance company and who share in any profits or losses. Officers are elected by the stockholders and manage stock insurance companies. Traditionally, stock companies issue nonparticipating policies, in which policyowners do not share in profits or losses. A nonparticipating (stock) policy does not pay dividends to policyowners; however, taxable dividends are paid to stockholders. The dividends are not guaranteed as they are based on company profit.
-
Mutual companies are owned by the policyowners and issue participating policies. With participating policies, policyowners are entitled to dividends, which, in the case of mutual companies, are a return of excess premiums and are, therefore, nontaxable. Dividends are generated when the premiums and the earnings combined exceed the actual costs of providing coverage, creating a surplus. Dividends are not guaranteed.
4. Fraternals A fraternal benefit society is an organization formed to provide insurance benefits for members of an affiliated lodge, religious organization, or fraternal organization with a representative form of government. Fraternals sell only to their members and are considered charitable institutions, and not insurers. They are not subject to all of the regulations that apply to the insurers that offer coverage to the public at large. In most states, fraternal benefit societies are permitted to issue life insurance (including endowments), health insurance (including medical and disability), and annuities. They do not issue property or liability policies.
5. Authorized and Unauthorized Companies and Certificate of Authority Before insurers may transact business in a specific state, they must apply for and be granted a license or Certificate of Authority from the state department of insurance and meet any financial (capital and surplus) requirements set by the state. Insurers who meet the state's financial requirements and are approved to transact business in the state are considered authorized or admitted into the state as a legal insurer. Those insurers who have not been approved to do business in the state are considered unauthorized or nonadmitted. Most states have laws that prohibit unauthorized insurers from conducting business in the state, except through licensed excess and surplus lines brokers.
Know This! Insurers must obtain a Certificate of Authority prior to transacting business in this state.
To conduct business in Arkansas, an insurer must receive a Certificate of Authority from the Department of Insurance. A Certificate of Authority indicates that the insurer has met the standards established by the Department and is qualified to make insurance transactions in Arkansas. Unless waived by the Commissioner, a foreign insurer must provide the Commissioner with evidence that it has been actively engaged in the insurance industry in its incorporated state for at least 3 years prior to the date of the application to do business in this state. This requirement does not apply to subsidiaries of insurers authorized to business in Arkansas, or mergers or consolidations with insurers authorized to do business in this state for at least 3 years prior to application. A Certificate of Authority cannot be issued to an insurer which is owned or controlled by any domestic or foreign government, political subdivision, instrumentality, or agency.
B. Insurance Commissioner The Insurance Commissioner is appointed by the Governor, with the advice and consent of the Senate. The Commissioner must be a citizen of Arkansas and at least 30 years of age. At the time of taking office, the Commissioner must execute a bond to the State of Arkansas in the sum of $50,000 for the faithful performance of the Commissioner's duties.
1. General Duties and Powers The Commissioner will enforce the provisions of the Insurance Code and execute the duties expressly conferred upon him or her by or reasonably implied from the provisions of the Arkansas Insurance Code. The Commissioner is authorized to enter into cooperative agreements with other governmental agencies inside and outside the state to regulate the business of insurance, including, but not limited to the following:
- Licensing of insurance companies;
- Licensing of insurance producers;
- Regulation of premium rates and policy forms;
- Regulation of insurer insolvency and insurance receiverships; and
- Other matters relating to the effective regulation of the business of insurance.
Examination of Books and Records The Commissioner regulates insurance companies authorized to do business in this state. The purpose of the examination of insurers' books and records is to ensure that the companies remain solvent and conduct business in compliance with state laws and regulations pertaining to licensing, policy forms, rates, claims, and market conduct. The Commissioner conducts examinations of insurance matters as authorized by the Insurance Code. Every domestic insurer may be examined when they apply for their initial certificate of authority or whenever the Commissioner deems appropriate. Examinations must be conducted at least once every 5 years. In addition to the examinations expressly authorized, the Commissioner may further examine any person to determine whether or not they have violated any provision of the Arkansas Insurance Code. Each person examined must pay to the State Insurance Department the actual travel expenses, reasonable living expense allowance, and compensation for examiners and other persons assisting in the examination.
2. Hearings, Notice of Hearings, and Orders Because the Commissioner's role is to enforce insurance laws and to protect the public from unfair trade practices, if the Commissioner suspects that an insurer or its agent has committed a violation or is engaged in an unfair trade practice, the Commissioner may issue a statement of charges and hold a hearing for any purpose deemed necessary (within the scope of the Insurance Code). Every order of the Commissioner must state its effective date, as well as its intent or purpose, the grounds on which the order is based, and the provisions of the Insurance Code pursuant to which action is taken. An aggrieved person may also demand a hearing, in which case, the Commissioner must schedule a hearing to be held within 30 days of receiving the request, unless the parties agree to postpone it. Once a hearing is scheduled, the Commissioner must give 10 days' notice to all parties affected by the hearing. The notice must provide the time and place of the hearing, as well as the content of the hearing. After the Commissioner makes a ruling, parties involved have 30 days to appeal the decision. Any request for additional arguments or a rehearing must be made in writing to the Commissioner, who may choose to reopen the matter. Within 30 days of the end of the hearing, the Commissioner must give a copy of the order on the hearing to the parties involved. The order must state the facts and the matters resolved by the hearing. Any party to the hearing may appeal the Commissioner's order within 30 days of receiving the order. In general, these procedural requirements also apply to hearings involving allegations of unfair trade practices. If the allegations are proven at a hearing, the Commissioner may order the person or insurer to cease and desist from committing the unfair or deceptive trade practice.
3. Penalties Any violation of the Insurance Code may result in a suspension or revocation of a license or certificate of authority. If a licensee is convicted of a crime as a result of violating the Insurance Code, the Commissioner may impose a fine of up to $1,000 per violation (not to exceed an aggregate penalty of $10,000). If a person commits a violation willfully and knowingly, the penalty is $5,000 for each act or violation (not to exceed a total of $50,000 in a 6-month period). A person who violates a cease and desist order of the Commissioner will be subject to a monetary penalty of up to $10,000 for each violation, or suspension or revocation of license.
C. Licensing
Insurance professionals must be properly licensed for a specific line of authority in order to transact insurance. The purpose of licensing is to ensure that a producer meets educational and ethical standards required to fulfill producer's responsibilities to the insurer and to the public. Licensing regulations set out the requirements, procedures, and fees relating to the qualification, licensure, and appointment of insurance producers.
1. Persons Required to be Licensed
To transact insurance as producers (agents or brokers), counselors, or adjusters, individuals must be properly licensed. Applicants for an insurance producer license or a consultant license (except temporary licenses), must do the following:
- Pass a written examination;
- Complete 20 hours of prelicensing classroom or online instruction for each line of insurance for which a license is sought, including at least 5 hours on the licensing of producers and the regulatory laws of the state; and
- Pay a licensing fee.
Producer A producer is a person required to be licensed under the laws of this state to sell, solicit, or negotiate insurance. To obtain a license as a producer or broker, the applicant must have complied with the Producer Licensing Model Act. In addition to the qualifications previously stated, candidates must
- Be at least 18 years of age; and
- Have not committed any act that is grounds for denial or revocation of the license. An insurance producer license will remain in effect unless revoked or suspended as long as all fees are paid and continuing education requirements for resident producers are met by the due date. A licensed insurance producer who is unable to comply with license renewal procedures due to military service or some other extenuating circumstance may request a waiver of those procedures. If an applicant for an insurance producer license in Arkansas was previously licensed for the same lines of authority in another state, the applicant will not be required to complete any prelicensing education or examination. This exemption is only available if the person is currently licensed in that state or if the application is received within 90 days of the cancellation of the applicant's previous license and if the prior state issues a certification that, at the time of cancellation, the applicant was in good standing in that state.
Consultant An insurance consultant is an individual, firm, limited liability company, or corporation that advises others about their insurance needs and coverages for a fee. If all the other prelicensing requirements are met, the Commissioner may issue an insurance consultant's license to any person who meets the following requirements:
- Is of legal age of majority or has had the status of minority removed for all general purposes;
- Has been a resident of Arkansas, or a town that is within the borders of Arkansas, for 30 days;
- Is appointed by an authorized insurer; and
- Is competent, trustworthy, financially responsible and of good character. All insurance consultants' licenses continue in force unless nonrenewed, expired, suspended, revoked or terminated, and are subject to annual continuation fee and a written request for license continuation to the Insurance Commissioner.
Resident and Nonresident To become a resident producer in this state, an individual must do the following:
- Either live or have a primary place of business in this state;
- Complete required prelicensing education;
- Pass the proper examination. To receive a nonresident producer license, a person must
- Be licensed as a resident in good standing in his or her home state;
- Have submitted the proper request for licensure and paid the fees required by the Insurance Code;
- Have submitted to the Commissioner the application for licensure that person submitted to his or her home state or a completed Uniform Application;
- Live in a state that awards nonresident producer licenses to residents of Arkansas on the same basis.
Temporary License The Commissioner may issue a temporary insurance producer license for a period of up to 180 days without requiring an examination if the temporary license is deemed necessary for the servicing of the existing insurance business in the following cases:
- To the surviving spouse or court-appointed representative of a licensed producer who dies or becomes mentally or physically disabled to allow adequate time for the sale of an insurance business owned by the producer or for the recovery of the producer to the business or to provide for the training and licensing of new personnel to operate the business;
- To the designee of a licensed producer entering active service in the armed forces of the United States of America; or
- In any other circumstance where the Commissioner deems that the public interest will best be served by the issuance of this license. The Commissioner may limit the authority of any temporary licensee to protect the insureds and the public. A temporary license may not continue after the owner or the personal representative disposes of the business.
2. Exemptions and Exceptions An insurance producer license is not required of any officer, director, or employee of an insurer organizations employed by the insurer, provided they are not directly or indirectly involved with the actual sale of insurance contracts, and do not receive any commission. Furthermore, the following persons are exempt from the licensing requirements:
- An officer or employee of an insurer who performs mainly executive, managerial or clerical duties;
- A person who secures and furnishes information for the purpose of enrolling individuals under group insurance policies or annuities, or issues certificates under group plans;
- Employers who execute a program of employee benefits for the employer's own employees;
- Insurer employees who inspect, rate, or classify risks, or supervise the training of insurance producers and who are not individually engaged in the sale, solicitation, or negotiation of insurance;
- A person whose activities are limited to advertising;
- A salaried full-time employee who advises his or her employer about the employer’s insurance interests; or
- Employees of an insurer who respond to requests from existing policyholders on existing policies and are not compensated based on premiums that result from these services and they do not sell, solicit, or negotiate insurance.
3. Producer Appointment and Termination of Contract An insurance producer must be appointed by an insurer before he or she can act as an agent of that insurer. To appoint a producer, an insurer must file a notice of appointment with the Commissioner within 15 days of the date the agency contract is executed or the first insurance application is submitted. Upon receipt of the notice of appointment, the Commissioner has 30 days to verify that the insurance producer is eligible for appointment. If the producer is ineligible for appointment, the Commissioner has 5 days to notify the insurer. If an insurer terminates the appointment of a producer, it must notify the Insurance Commissioner within 30 days of the effective date of the termination.
4. Maintaining a License
Continuing Education Continuing education rules are established to protect the public by maintaining high standards of professional competence in the insurance industry, and to maintain and improve the insurance skills and knowledge of licensed producers. As a condition for continuation of their licenses, insurance producers licensed in Arkansas must complete 24 hours of continuing education (CE) courses every 2 years. At least 3 hours of CE hours must be in ethics. Arkansas CE requirements do not apply to:
- A person holding a license for any kind of insurance that doesn't require an examination;
- Limited or restricted licenses exempt by the Commissioner;
- A person who is at least 60 years of age;
- A person who has held an active license for at least 15 consecutive years;
- A licensee that is a firm, limited liability company, or corporation;
- Nonresident producers;
- Limited insurance consultants;
- A nonresident licensee in the first full year of resident licensing following a change of domicile or residency to Arkansas;
- A member of the Arkansas National Guard or United States Armed Forces on active duty.
Change of Name and Address A licensee must notify the Commissioner of a change of legal name or address within 30 days of the change. Any changes of the address of the place of business must be reported to the Commissioner within 10 days. Administrative Fees If the Commissioner finds that any grounds exist for the suspension or revocation of any license, the Commissioner may impose upon the licensee an administrative penalty of up to $1,000 per violation. Willful misconduct or willful violation on the part of the licensee may be subject to a fine up to $5,000 per violation.
5. Renewal, Suspension, or Revocation of License
In order to renew a license, newly licensed agents or brokers can wait until the first annual period after the first renewal of their license. The licenses will expire on the last day of the licensee's birth month. An insurance producer or consultant who allows his or her license to lapse may reinstate the license without passing a written examination within 12 months of the due date. A penalty of double the unpaid renewal fee will be required for any renewal fee received after the due date. The Commissioner may suspend for up to 36 months, revoke, refuse to continue, or place on probationary status any license if any of the following causes exist:
- Providing incorrect, misleading, or materially untrue information in the license application;
- Violating any insurance law, regulation, or order;
- Obtaining or attempted to obtain a license through misrepresentation;
- Improperly withholding, misappropriating, or converting any moneys or properties received in the course of doing insurance business;
- Intentionally misrepresenting the terms of an actual or proposed insurance contract;
- Having been convicted of a felony;
- Committing an insurance unfair trade practice or fraud;
- Using fraudulent, coercive or dishonest practices in the conduct of the business of insurance;
- Having an insurance license denied, suspended or revoked in any other state;
- Forging another's name to an application of insurance or other document;
- Knowingly accepting insurance business from an unlicensed individual;
- Failing to comply with an administrative or court order imposing child support; or
- Failing to pay state income tax. All licenses are the property of the state of Arkansas. Upon license expiration, termination, suspension or revocation, the licensed producer must immediately deliver the license to the Insurance Commissioner either by personal delivery or by mail. Producers who terminate their state residence must deliver the insurance license to the Commissioner within 10 days after terminating their residency.
D. Producer Responsibilities
1. Fiduciary Capacity The producer is legally obligated to perform in an ethical manner. An insurance producer who agrees to obtain coverage for a client is obligated to exercise the same degree of care as would be expected from a reasonable, prudent, and competent professional in the field. This responsibility is referred to as the producer's fiduciary responsibility. A fiduciary is a producer who handles insurer funds in a trust capacity. He or she does not commingle premiums collected with his or her own personal funds. If failure to exercise this degree of care results in a loss to a client, the producer may be held liable for that loss. Producers have been held liable for both negligence and breach of contract with respect to clients in numerous areas. All funds, premiums, or return of premiums received by a licensee in the capacity as a licensee will be received in a fiduciary capacity, and the licensee must account for and pay these funds to the insurer, insured or any other person entitled to them. Any licensee who diverts or appropriates the funds will, upon conviction, be found guilty of theft of property and punished as provided by law.
2. Commissions Insurers cannot pay commissions or any other compensation for services unless the producer was properly licensed when the services were performed. A person cannot accept commissions for services if he or she is not properly licensed. Former producers may receive renewal or other deferred commissions if they were properly licensed at the time of the transaction. Commissions may be assigned to an insurance agency or people who do not sell, solicit, or negotiate insurance in this state as long as it would not be considered a rebate or any other violation of insurance laws.
3. Fraud Reporting Anyone engaged in the business of insurance who knows about a fraudulent insurance act must inform the Commissioner. Failing to report this information is considered a Class A misdemeanor. While investigating a fraudulent act or related violation, the Commissioner may request information from any producer. Refusing to comply with this request is grounds for the suspension, revocation, denial or nonrenewal of that producer’s license.
E. Marketing Practices
1. Unfair Claims Practices
In Arkansas, it is improper claims settlement practice for a domestic, foreign, or alien insurer to commit any of the following acts flagrantly or with such frequency as to indicate a general business practice:
- Knowingly misrepresenting relevant facts or policy provisions to claimants or insureds.
- Failing to acknowledge communications regarding claims arising under its policies (within 15 working days).
- Failing to adopt and implement procedures for the prompt investigation and settlement of claims arising under its policies.
- Not attempting in good faith to bring about prompt, fair, and equitable settlement of claims submitted in which liability has become reasonably clear.
- Compelling insureds or beneficiaries to institute suits to recover amounts due under their policies by offering substantially less than the amount ultimately recovered in suits brought by them.
- Refusing to pay claims without conducting a reasonable investigation.
- When requested by the insured in writing, failing to affirm or deny coverage of claims within a reasonable time after completing an investigation related to the claim.
- When requested by the insured in writing, making claims payments to an insured or beneficiary without indicating the coverage under which each payment is being made.
- Unreasonably delaying the investigation or payment of claims by requiring both a formal proof of loss and subsequent verification that duplicates the information.
- When requested by the insured in writing, failing in the case of claims denial or offer of compromise settlement to provide a prompt explanation of the basis for such action.
- Failing to provide forms necessary to file claims within 20 calendar days of a request, with a reasonable explanation regarding their use.
- Issuing checks or drafts in partial settlement of a loss or claim under a specific coverage which contains language that releases the insurer or its insured from its total liability.
Upon receipt of any inquiry from the Arkansas Insurance Department regarding a claim, insurers must provide the Department with a reasonably adequate response within 15 working days of the inquiry.
Insurers are required to complete the investigation of a claim within 45 calendar days after notification of a claim. If the investigation cannot be reasonably completed within 45 days, the insurer must notify the claimant that additional time is required and include the reasons for the delay.
Insurers must mail or deliver claim checks to claimants within 10 working days after the claims are processed, all claim investigations are completed, and the claim files are closed and ready for payment.
2. Unfair Methods of Competition
Insurers and insurance producers may not engage in any trade practice that is defined as, or determined to be, an unfair method of competition or an unfair or deceptive act or practice in the business of insurance.
It is considered an unfair trade practice to knowingly engage in an unfair method of competition with enough frequency that the commission of unfair marketing practices indicates a general business practice.
If, after a hearing, the Department determines that a producer or an insurer has committed an unfair trade or competition practice, the Department may issue an order requiring the person to cease and desist from engaging in the method of competition, act, or practice, and/or impose penalties for violation of insurance laws.
Misrepresentation
It is illegal to issue, publish, or circulate any illustration or sales material that is false, misleading, or deceptive as to policy benefits or terms, or the payment of dividends. This also refers to verbal statements. Committing this illegal act is called misrepresentation.
Any person who violates state statutes regarding misrepresentation of policies, if convicted, will be found guilty of a Class D felony and will be punished by:
- A fine of up to $10,000.
- Imprisonment in the state penitentiary for up to 6 years.
- Both fine and imprisonment.
False Advertising
Advertising covers a wide scope of communication, from publishing an ad in a newspaper or magazine to broadcasting a commercial on television or the Internet. Advertisements cannot include any untrue, deceptive, or misleading statements that apply to the business of insurance or anyone who conducts it. The violation of this rule is called false advertising.
It is prohibited to advertise or circulate any materials that are untrue, deceptive, or misleading. False or deceptive advertising specifically includes misrepresenting any of the following:
- Terms, benefits, conditions, or advantages of any insurance policy.
- Any dividends to be received from the policy or previously paid out.
- Financial condition of any person or the insurance company.
- The true purpose of an assignment or loan against a policy.
- Representing an insurance policy as a share of stock, or using names or titles that may misrepresent the true nature of a policy also will be considered false advertising. In addition, a person or an entity cannot use a name that deceptively suggests it is an insurer.
False Financial Statements
False financial statements are those that are intended to deceive public officials or the general public about the financial condition of an insurer. This often occurs when an important fact about the financial status of an insurer is deliberately withheld to present the company in a more favorable light.
Rebating
Rebating is defined as any inducement offered to the insured in the sale of insurance products that is not specified in the policy. Both the offer and acceptance of a rebate are illegal. Rebates may include, but are not limited to the following:
- Rebates of premiums payable on the policy.
- Special favors or services.
- Advantages in the dividends or other benefits.
- Stocks, bonds, securities, and their dividends or profits.
Twisting
Twisting is a misrepresentation, incomplete, or fraudulent comparison of insurance policies that persuades an insured/owner, to their detriment, to cancel, lapse, switch policies, or take out a policy with another insurer. Twisting is prohibited.
Churning of Business
Churning is defined as replacing insurance policies for the sole purpose of making commissions. The original policy values are used to purchase another insurance with the same insurer for the purpose of earning additional premiums, fees, or commissions. It is illegal to replace existing life or disability policies with new policies if the producer cannot demonstrate that the replacement will benefit the insured.
Defamation
Defamation occurs when an oral or written statement is made that is intended to injure a person engaged in the insurance business. This also applies to statements that are maliciously critical of the financial condition of any person or a company.
Boycott, Coercion, and Intimidation
It is illegal to be involved in any activity of boycott, coercion, or intimidation that is intended to restrict fair trade or to create a monopoly. This would include unfair behavior that influences not only clients but competing agents and brokers. Coercion is to require, as a condition of a loan, that the applicant purchase insurance from a specific insurer.
Unfair Discrimination
Discrimination in rates, premiums, or policy benefits for persons within the same class or with the same life expectancy is illegal. No discrimination may be made on the basis of an individual's marital status, race, national origin, gender identity, sexual orientation, creed, or ancestry unless the distinction is made for a business purpose or required by law.
3. Advertising: Producer Responsibilities
First and foremost, advertising must be accurate and not misrepresent the facts. Advertising rules apply to any insurance advertisement intended for presentation, distribution, dissemination, or other advertising use when used or made either directly or indirectly by or on behalf of the insurance company.
Every insurance company must establish and maintain a system of control over the content, form, and method of dissemination of all advertising of its policies. The insurer whose policies are advertised is responsible for all its advertisements, regardless of who wrote, created, presented, or distributed them.
Advertising includes any material designed to create public interest in an insurance product or company or to induce members of the public to purchase, increase, or modify an insurance policy. An advertisement may take any of the following forms:
- Printed and published material.
- Audio/visual material.
- Mailing envelopes and descriptive literature used in direct mailings.
- Newspaper, magazine, television, billboards, and similar displays.
- Prepared sales talks, presentations, and materials used by the companies' sales personnel or other paid celebrities. The use of celebrities or third party endorsements must be genuine, represent the author's current opinion, be applicable to the policy, and be accurately reproduced. If the person making the testimonial has a financial interest in the insurer, it must be stated, and if the endorser was paid, the words "paid endorsement" must appear in the ad.
The form and content of all advertisements must be clear enough to avoid deception (as determined by the Commissioner). Advertisements must not use the words investment, profits, or other similar phrases that might mislead a purchaser into believing that they may receive something that is not available to other persons of the same class and life expectancy, unless it is the truth. They also must not use the phrases nonmedical, no medical examination required, or similar phrases unless the policy is a guaranteed issue policy not dependent on answers to health questions.
Regarding the advertising of insurance policies, insurers cannot make, issue, or circulate any estimate, illustrations, statement, or sales presentation that:
- Misrepresents the benefits, advantages, conditions, or terms of any insurance policy.
- Misrepresents the dividends or share of the surplus to be received on any insurance policy.
- Makes any false or misleading statements about the dividends or share of surplus previously paid on any insurance policy.
- Is misleading or is a misrepresentation as to the financial condition of any person or as to the legal reserve system upon which any life insurer operates.
- Uses any name or title of any insurance policy or class of insurance policies, misrepresenting the true nature thereof.
- Is a misrepresentation for the purpose of inducing or tending to induce the lapse, forfeiture, exchange, conversion, or surrender of any insurance policy.
- Is a misrepresentation for the purpose of effectuating a pledge or assignment of or effecting a loan against any insurance policy.
- Misrepresents any insurance policy as being shares of stock.
Insurance companies must keep files of all advertisements used in Arkansas and must note the manner and extent of distribution and the form number of any advertised policy. These files are subject to inspection by the Insurance Department and must be kept either for 4 years or until the next regular examination by the Insurance Department. All insurers must file a certificate of compliance with their annual statement, stating that their advertisements comply with Arkansas regulations.
F. Life and Health Insurance Guaranty Association Act
The Arkansas Life and Health Insurance Guaranty Association was established to protect policyowners, insureds, and beneficiaries of policies issued by insurers who become insolvent or are unable to perform their contractual obligations. All insurers must be members of the Association as a condition of their authority to transact insurance in the state. All authorized insurers contribute to a fund to provide for the payment of claims for insolvent insurers. The Association's board of directors consists of between 5 and 9 members, selected by members and supervised by the Commissioner.
The Association covers direct life and disability insurance policies and supplemental contracts. In the event of a member insurer's insolvency, the Association is liable for no more than the contractual obligation the insurer would have held if it had not become insolvent. Liability cannot amount to more than $300,000 for any one life in:
- Life insurance benefits.
- Disability benefits.
- Annuity benefits.
The Association does not cover the following:
- The portion of a variable life insurance or variable annuity contract not guaranteed by an insurer.
- The portion of any policy or contract under which the risk is borne by the policyholder.
- Any policy or contract assumed by the impaired or insolvent insurer under a reinsurance contract without assumption certificates.
- Any policy, contract, or subscriber agreement issued by a nonprofit hospital service corporation.
- A policy issued by a fraternal benefit society.
- A group policy issued by an employer, association, or other entity.
It is an unfair trade practice to make any statement that an insurer's policies are guaranteed by the existence of the Insurance Guaranty Association.
Know This! Insurers cannot advertise protection by the Insurance Guaranty Association.
G. By The Numbers - Summary Chart
In order to perform your best on the state regulations portion of the exam, make sure you memorize these numbers and their definitions.
Department of Insurance Regulations:
- 4 years: Commissioner's term of office.
- 5 years: Examination of insurers.
- 30 days: Commissioner must grant a hearing to those aggrieved by insurance matters.
- 10 days: Amount of notice that all parties to the hearing must receive.
- 30 days: To appeal the Commissioner's decision.
- 30 days: After the hearing for the Commissioner to give a copy of the order to all parties.
- 3 years (36 months): Maximum suspension period for an insurance license.
Licensing and Appointment Requirements:
- 18 years: Minimum age to apply for a license.
- 180 days: Maximum duration of a temporary license.
- 12 months: To reinstate a license after it lapses without retaking the state exam.
- 15 days: For an insurer to file a notice of appointment.
- 30 days: For an insurer to file a notice of termination of appointment.
Miscellaneous Producer Regulations:
- 24 hours: Continuing education requirement per licensing period.
- 3 hours: Ethics continuing education requirement per licensing period.
- 2 years: The licensing period for insurance licenses.
- 30 days: To report a change of name or address.
Important Dollar Amounts:
- $1,000: For each violation of the Insurance Code (limited to $50,000 in a 6-month period).
- $1,000: Maximum penalty for violations that result in a suspended license.
- $5,000: Maximum penalty for intentional violations that result in a suspended license.
- $300,000: Guaranty Association's limit in covering individual claims.
H. Chapter Recap
This chapter focused on state-specific regulations for insurers and producers. Let's recap some of the important requirements and processes:
STATE REGULATIONS
-
Commissioner of Insurance:
- Appointed by the Governor for 4 years.
- Regulates the internal affairs of the Department of Insurance.
- Does not write laws.
- Examines all authorized insurers (once every 5 years).
-
Producer Regulation:
- Only one license of the same type is allowed per agent.
- Must be licensed in the line of authority for which the agent transacts insurance.
- Must be appointed to represent an insurer.
- Avoid unfair trade practices.
-
Insurance Company Regulations:
- Domicile - domestic, foreign, alien.
- Must be authorized - Certificate of Authority.
- Appoint producers to represent the insurer.
- Avoid unfair methods of competition and unfair claim settlements.
- Must be a member of the state Insurance Guaranty Association.
LICENSING REQUIREMENTS
-
Licensing Process:
- Minimum age requirement (18 years old).
- Meet prelicensing education requirement.
- Pass examination.
- Submit application and fees.
- Be of good character.
- Have not committed any violations that are grounds for license denial.
-
Types of Licenses:
- Individuals - resident and nonresident.
- Temporary license - valid for 180 days; issued to maintain the existing business.
-
Maintenance and Duration:
- Must be renewed every 2 years.
- Continuing education - must be completed every reporting period.
- Report changes of name or residential address and administrative actions or criminal prosecutions within 30 days; report change of business address within 10 days.
- License is not required if a person does not receive commissions.
- Disciplinary actions:
- Suspension, revocation, or refusal to renew a license.
- Cease and desist order.
- Monetary fines.
- Imprisonment.
Important Dollar Amounts:
- $1,000: For each violation of the Insurance Code (limited to $50,000 in a 6-month period).
- $1,000: Maximum penalty for violations that result in a suspended license.
- $5,000: Maximum penalty for intentional violations that result in a suspended license.
- $300,000: Guaranty Association's limit in covering individual claims.
H. Chapter Recap
This chapter focused on state-specific regulations for insurers and producers. Let's recap some of the important requirements and processes.
STATE REGULATIONS
Commissioner of Insurance
- Appointed by Governor for 4 years
- Regulates the internal affairs of the Department of Insurance
- Does not write laws
- Examines all authorized insurers (once every 5 years)
Producer Regulation
- Only one license of the same type is allowed per agent
- Must be licensed in the line of authority for which the agent transacts insurance
- Must be appointed to represent an insurer
- Avoid unfair trade practices
Insurance Company Regulations
- Domicile - domestic, foreign, alien
- Must be authorized - Certificate of Authority
- Appoint producers to represent the insurer
- Avoid unfair methods of competition and unfair claim settlements
- Must be a member of the state Insurance Guaranty Association
LICENSING REQUIREMENTS
Licensing Process
- Minimum age requirement (18 years old)
- Meet prelicensing education requirement
- Pass examination
- Submit application and fees
- Be of good character
- Have not committed any violations that are grounds for license denial
Types of Licenses
- Individuals - resident and nonresident
- Temporary license - valid for 180 days; issued to maintain the existing business
Maintenance and Duration
- Must be renewed every 2 years
- Continuing education - must be completed every reporting period
- Report changes of name or residential address and administrative actions or criminal prosecutions within 30 days; report change of business address within 10 days
- License is not required if a person does not receive commissions
- Disciplinary actions:
- Suspension, revocation, or refusal to renew a license
- Cease and desist order
- Monetary fines
- Imprisonment
-
Arkansas Statutes, Rules & Regulations pertinent to Health Only
Arkansas Statutes, Rules & Regulations pertinent to Health OnlyArkansas Statutes, Rules, And Regulations Pertinent To Health Only
There are insurance regulations in this state that apply only to Health insurance policies. This section explains some of these laws, including state programs and organizations that serve the insured.
TERMS TO KNOW
- Blanket policy — covers members of a particular group when they are participating in a particular activity, without naming individual insureds (such as students, passengers, sports teams)
- Claimant — a person who submits a claim for payment of benefits
- Dependent — someone relying on the insured for support
- Disclosure — information revealed to help someone make an informed and educated decision
- Guaranteed renewable — a policy written on a noncancellable basis with the guaranteed right to renew
- NAIC — National Association of Insurance Commissioners, a standard-setting and regulatory support organization governed by the chief insurance regulators from the 50 states, the District of Columbia and U.S. territories
- Nonrenew — terminate an insurance policy at its expiration date
- Solicitation — an attempt to persuade a person to buy an insurance policy, and it can be done orally or in writing
A. Policy Provisions
- Policy Requirements
All disability (health) insurance policies issued in Arkansas must be printed clearly in 10-point type and include:
- The entire premium for the policy;
- The dates when the insurance begins and ends;
- Exceptions and reductions of indemnity in either the benefit provision to which they apply or under a heading such as Exceptions or Exceptions and Reductions; and
- A form number in the lower left-hand corner of the first page (this applies to riders and endorsements as well).
Health policies can only insure one person, plus the insured's spouse and dependents, and may not include any portion of an insurer's charter, rules, or bylaws.
Unless rejected in writing by an insured, no accident and health insurance policy that provides coverage for inpatient services may be issued in Arkansas unless the following outpatient services are covered on the same basis:
- Laboratory and pathological tests;
- X-rays;
- Chemotherapy;
- Radiation treatment; and
- Renal dialysis.
Every accident and health policy delivered in Arkansas must contain the following provisions:
- Entire contract — The policy, including the endorsements and the attached papers, if any, constitutes the entire contract.
- Time limit on certain defenses — After a policy has been in force for 3 years, no misstatements, except fraudulent misstatements, made by the applicant, can be used to void the policy or to deny a claim.
- Grace period — This provision establishes a period of time after the premium due date that the policyowner has to pay the premium before the policy lapses. The length is based on the how often premiums are paid (7 days for weekly premium policies, 10 days for monthly premium policies and 31 days for all other policies).
- Reinstatement — If a renewal premium is not paid within the time allowed, a subsequent acceptance of premium by the insurer or an agent will reinstate the policy.
- Notice of claim — Written notice of claim must be given to the insurer within 20 days of the occurrence of a loss covered by the policy.
- Claim forms — The insurer, upon receipt of a notice of claim, must furnish claim forms to the claimant within 15 days.
- Proofs of loss — Written proof of a continuing loss must be given to the insurer within 90 days after the termination of the period for which the insurer is liable.
- Time of payment of claims — Benefits payable under this policy must be paid immediately upon receipt of due written proof of such loss.
- Payment of claims — Indemnity for loss of life will be payable according to the beneficiary designation. If no beneficiary designation is effective, such indemnity will be payable to the estate of the insured. All other indemnities will be payable to the insured.
- Physical examination and autopsy — The insurer (at its own expense) has the right and opportunity to examine the insured during a claim and, where not prohibited by law, to perform an autopsy on a deceased insured.
- Legal actions — A lawsuit to seek benefits on a policy cannot be filed until more than 60 days after written proof of loss has been provided, but must be filed within 3 years of providing proof of loss.
- Change of beneficiary — Unless the insured makes an irrevocable designation of beneficiary, the insured reserves the right the change the beneficiary without the consent of the beneficiary.
Arkansas has established the following as Minimum Standards for Benefits:
- A noncancellable, guaranteed renewable, or noncancellable and guaranteed renewable policy cannot terminate coverage for the spouse for any reason other than nonpayment of premium. The policy must provide that if the insured dies, the spouse of the insured, if covered, becomes the insured.
- The words noncancellable, guaranteed renewable, or noncancellable and guaranteed renewable must be defined in the policy and may only be used in a policy in which the insured has the right to continue until age 65 or until eligible for Medicare.
- In a family policy covering both husband and wife, the age of the younger spouse must be used as the basis for meeting age and duration requirements.
When accidental death and dismemberment is part of the insurance coverage, the insured has the option to include any covered dependent and not just the principal insured.
If the policy contains a provision that suspends coverage during military service, the policy must refund the applicable premium on a pro rata basis.
If an insurer cancels or refuses to renew a policy that provides pregnancy benefits, it must provide for an extension of those benefits.
Policies providing convalescent or extended care benefits following hospitalization cannot condition those benefits upon being admitted to the convalescent facility within 14 days of being discharged from the hospital.
Family coverage will continue for any unmarried dependent child who is incapable of self-sustaining employment due to mental retardation or physical handicap beyond the child's attaining the age of 19.
Any policy may contain a provision relating to recurrent disabilities, provided that no such provision specifies that a recurrent disability be separated by a period of greater than 6 months.
Any policy coverage for the recipient in a transplant operation will also provide reimbursement of any medical expenses of a live donor if benefits remain and are available under the recipient's policy.
Disability income benefits, if provided, cannot require the loss to begin less than 30 days after the accident, nor can any policy that the insurer cancels or refuses to renew require that it be in force at the time the disability occurred.
If, to prevent overinsurance, benefits are reduced due to the presence of Medicare, then benefits may be reduced for those insureds actually covered by Medicare. Benefits may not be reduced based solely on eligibility for Medicare.
Dollar limits from medical, accident, confinement, special care coverage offered by insurers in Arkansas are all set by regulation.
An individual health benefit plan must be renewable at the option of the insured, except for:
- Nonpayment of premium;
- Fraud or intentional misrepresentation by the insured;
- An insured no longer resides, lives, or works in the service area for which the insurer is authorized to do business;
- Election by the insurer to nonrenew a particular or all health benefit plans delivered or issued to individuals in Arkansas; and/or
- Individual termination of membership in an association receiving coverage.
If an insurer elects to discontinue offering a particular health benefit plan, it must provide notice of discontinuation to all affected insureds at least 90 calendar days prior to the date the health benefit plan will be discontinued by the carrier.
Insurers must offer the insureds the option to purchase other health benefit plans on a guaranteed issue basis. The decision to discontinue cannot be on the basis of any health-related factor of an insured.
If an insurer elects to nonrenew all of its health benefit plans, the insurer is required to provide advance notice of its decision to the Commissioner and all affected insureds at least 180 calendar days prior to nonrenewal.
An insurer that elects not to renew a health benefit plan will be prohibited from writing new business in the individual market in this state for a period of 5 years from the date of discontinuation.
An insurer is not prohibited from modifying coverage at the time of coverage renewal, as long as the modification is consistent with state law and is made on a uniform basis among all insureds covered under a similar policy.
2. Coverages Coverage for Newborns
All individual and group health insurance policies providing coverage for a family member of the insured must also provide coverage for a newborn child of the insured from the moment of birth. This includes coverage for injury or sickness, including the necessary care and treatment of medically diagnosed congenital birth defects and birth abnormalities. In addition, coverage for newborn infants must include routing nursery care and pediatric costs for a well newborn child for up to 5 full days in a hospital nursery or until the mother is discharged from the hospital, whichever is the shorter period.
Notification of the birth of the newborn child and payment of the required premium must be furnished to the insurance company within 90 days after the date of birth.
Coverage for Mental Health Services
All health insurance contracts must cover the treatment of mental disorders. This coverage must be at least as extensive as that provided for physical illnesses.
The insurer may establish a co-payment requirement for mental illness benefits paid for inpatient, partial hospitalization, or outpatient care that may differ from the co-payment requirements for any other covered illness.
The insurer may not impose different provisions for mental illness with regard to deductible amounts, lifetime maximum payments, payments per day of inpatients or outpatients.
Coverage for Maternity Benefits
Health care insurers may not restrict a hospital stay for the mother and a newborn child to less than 48 hours for a vaginal delivery and 96 hours for a cesarean section. The mother and newborn child may leave earlier if the attending physician and the mother both agree to the early departure.
Coverage for Chiropractic Services
An injured employee has the right to seek treatment from a chiropractor without first seeing a physician. The insured must prove the treatment is reasonable and necessary and casually related to his or her compensable injury.
Coverage for Substance Abuse
Each policy must provide a minimum benefit of $6,000 for each 24-month period, no more than half of which can be spent during any period of 30 consecutive days. Each recipient of these benefits is limited to a minimum lifetime amount of $12,000.
3. Advertising The Arkansas Insurance Department has established rules governing the advertisement of all health insurance policies except Medicare supplement insurance. These rules developed by the department establish guidelines as to what are permissible and impermissible standards of conduct in the advertising health insurance in order to prevent unfair, deceptive, and misleading advertising.
Every insurer must maintain a system of control at all times over the content, form, and method of all advertisements of its policies. All advertisements, regardless of who wrote, created, designed, or presented them, are the responsibility of the insurance company.
Words, phrases, statistics, or illustrations may not be used in a way that misleads or deceives consumers about policy premiums, benefits payable, or losses covered. Nor may advertisements use words or phrases known only to people who are familiar with insurance terminology.
Each advertisement must include the insurer's name.
No advertisement can contain or use words or phrases such as all, full, complete, comprehensive, unlimited, up to, as high as, this policy will help fill some of the gaps that Medicare and your present insurance leave out, the policy will help replace your income, or similar words and phrases that are meant to exaggerate the benefits of the policy.
Policies covering only specific diseases must state clearly the policy's limitations.
B. Medicare Supplement Make sure you review the Social Insurance chapter for information about Medicare Supplement Policies.
1. Minimum Standards
Medicare supplement policies and certificates must adhere to the National Association of Insurance Commissioners' standardized model Medicare supplement policy.
2. Provisions
Medicare supplement policies or certificates in force in Arkansas may not contain benefits that duplicate benefits provided by Medicare.
Medicare supplement policy or certificate may not exclude or limit benefits for losses incurred more than 6 months from the effective date of coverage because it involved a pre-existing condition. The policy cannot define a pre-existing condition more restrictively than a condition for which medical advice was given or treatment was recommended by or received from a physician within 6 months before the effective date of coverage.
The Commissioner may issue reasonable regulations to establish specific standards for policy provisions of Medicare supplement policies. These standards will be in addition to and in accordance with applicable laws of Arkansas. No requirement of Arkansas law relating to minimum required policy benefits, other than the minimum standards provided below, apply to Medicare supplement policies and certificates. The standards may cover, but not be limited to:
- Terms of renewability;
- Initial and subsequent conditions of eligibility;
- Nonduplication of coverage;
- Probationary periods;
- Benefit limitations, exceptions, and reductions;
- Elimination periods;
- Requirements for replacement;
- Recurrent conditions; and
- Definition of terms.
The Commissioner will issue reasonable regulations to establish minimum standards for benefits, claims payment, marketing practices, compensation arrangements, and reporting practices for Medicare supplement policies.
The Commissioner may issue reasonable regulations necessary to conform Medicare supplement policies to the requirements of federal law, including, but not limited to:
- Requiring refunds or credits if the policies or certificates do not meet loss ratio requirements;
- Establishing a uniform methodology for calculating and reporting loss ratios;
- Assuring public access to policies, premiums, and loss ratio information of issuers of Medicare supplement insurance;
- Establishing a process for approving or disapproving policy forms and certificate forms and proposed premium increases;
- Establishing a policy for holding public hearings prior to approval of premium increases; and
- Establishing standards for Medicare SELECT policies and certificates.
The Commissioner may issue reasonable regulations that specify prohibited policy provisions not otherwise specifically authorized by statute, which, in the opinion of the Commissioner, are unjust, unfair, or unfairly discriminatory to any person insured or proposed to be insured under a Medicare supplement policy or certificate.
3. Right to Return Medicare supplement policies must have a notice prominently printed on the first page of the policy stating that the applicant will have the right to return the policy within 30 days of its delivery and to have the premium refunded if the applicant is not satisfied for any reason. Any refund made must be paid directly to the applicant by the issuer in a timely manner.
4. Disclosure Standards With every Medicare supplement policy delivered in Arkansas, an outline of coverage must be provided to the applicant at the time of application. The format and content of the outline of coverage is determined by the Commissioner. The outline of coverage must include:
- A description of the principal benefits and coverage provided in the policy;
- A statement of the renewal provisions, including any reservation by the issuer of a right to change premiums, and disclosure of the existence of any automatic renewal premium increases based on the age of the policyholder or certificate holder; and
- A statement that the outline of coverage is a summary of the policy.
The Commissioner may establish rules regarding a Buyer's Guide for individuals eligible for Medicare, designed to improve the buyer's ability to select the most appropriate coverage. The Commissioner may require that a guide be provided to prospective insureds during the delivery of the outline of coverage or upon request by the prospective insured, but no later than during the delivery of the policy.
C. Long-Term Care Insurance Act
1. Coverage
Long-term care insurance is any policy or rider designed to provide coverage for diagnostic, preventive, therapeutic, rehabilitative or personal care services provided in a setting other than the acute care unit of a hospital. It is offered primarily to provide coverage for at least 12 consecutive months for each covered person.
No long-term care insurance policy can be delivered in Arkansas if it limits or excludes coverage by type of illness, treatment, medical condition, or accident. However, exclusions can be made for the following:
- Pre-existing conditions;
- Mental or nervous disorders, other than Alzheimer's disease;
- Alcoholism and drug addiction;
- Illness, treatment, or medical condition arising out of war or participation in a felony;
- Services provided outside the United States;
- Attempted suicide or intentional self-inflicted injury;
- Treatment in a government facility at no cost to the insured; or
- From service in the armed forces.
2. Minimum Standards
Long-term care insurance policies may not:
- Be canceled, non-renewed, or otherwise terminated on the grounds of the age or the deterioration of the mental or physical health of the insured individual;
- Contain a provision establishing a new waiting period in the event existing coverage is converted to or replaced by a new other form within the same company; or
- Provide coverage for skilled nursing care only or provide significantly more coverage for skilled care in a facility than coverage for lower levels of care.
3. Provisions
Applicants for LTC insurance have the right to return a policy within 30 days of its delivery for a full refund if not satisfied for any reason.
LTC policies may not define a pre-existing condition more stringently than a condition for which medical advice was sought within the past 6 months.
For LTC policies that have been in force for at least 6 months but less than 2 years, an insurer may rescind the policy or deny a claim upon showing of misrepresentation that is both material to the acceptance for coverage and pertains to the condition for which benefits are sought. However, once a policy has been in force for 2 years, the policy is not contestable upon the grounds of misrepresentation alone. The policy may be contested only upon a showing that the insured knowingly and intentionally misrepresented relevant facts relating to the insured's health.
No long-term care insurance policy may be delivered unless the policyholder, at the time of application, is offered the option of purchasing a policy that provides for nonforfeiture benefits to the defaulting or surrendering policyholder. The Commissioner will promulgate a regulation specifying the type or types of nonforfeiture benefits to be included in such policies and the standards for the benefits.
D. Group And Blanket Health
1. Standards
All benefits under blanket policies must be payable to the persons insured, their designated beneficiaries, or estate. If the insured is a minor, the benefits would be payable to a parent or guardian. Blanket policies are prohibited from requiring services be rendered by a particular hospital or person.
Any insurer authorized to offer disability insurance in Arkansas is also authorized to offer blanket disability coverage to the following groups:
- Common carriers, covering all passengers of the common carrier;
- Policies issued to any employer, covering a group of employees having exceptional hazards involved in their employment;
- Institutions of learning, covering students and teachers;
- Religious, charitable, recreational, educational, or civic organizations, covering any group of members or participants defined in the specified hazards incidental to any activity sponsored or supervised by the policyholder;
- Volunteer fire departments or similar volunteer groups;
- Sports teams or camps; and
- Any other type of group that the Commissioner deems qualified for blanket health policies.
Individual applications are not required of all insureds under a blanket policy. An insurer is not required to provide a certificate of coverage to each insured.
Any group must meet the following basic requirements to apply for group or blanket coverage:
- Articles of incorporation and bylaws;
- At least 100 members; and
- Have been in active existence for at least 2 years for purposes other than that of obtaining insurance.
2. Provisions
Group accident and health insurance policies issued in Arkansas must contain the following required provisions:
- In the absence of fraud, all statements made by applicants, the policyowner, or insured person are deemed representations and not warranties;
- No statement can void coverage or reduce benefits, unless a written disclosure is signed by the policyholder, and a copy of the disclosure is provided to the policyholder, insured, and/or beneficiary;
- Coverage cannot end for unmarried dependents of the insured who have reached the limiting age, but are incapable of self-sustainable employment due to a mental or physical disability and are dependent on the insured for support;
- Insurers must deliver a summary of essential policy features to each insured;
- Coverage may be extended to new eligible employees, members, or dependents;
- Group accident and health policies must provide outpatient coverage on the same basis and provide the same service as those under inpatient coverage, unless rejected in writing by the policyowner;
- Benefits must be payable immediately upon receipt of proof of loss and benefits for loss of time must be payable within 30 days of the period for which the insurer is liable;
- Every insurer, hospital or medical service corporation, fraternal benefit society, self-funded healthcare plan, or HMO providing replacement coverage must provide immediate coverage to employees and dependents within 60 days of discontinuance of a prior plan, as long as:
- Each employee or dependent was covered under the previous plan;
- Each employee or dependent is a member of the class of individuals eligible for coverage under the previous plan, regardless of plan limitations or exclusions relating to "actively at work" or hospital confinement; and
- The previous plan provided coverage to at least 15 members.
- Continuation of Coverage — Every group accident and health insurance policy, other than accident only or specified disease policies, must contain a provision that any certificate holder, member or spouse whose coverage under a policy would end due to the termination of employment, group membership, or change in marital status may continue coverage under the policy for themselves and any eligible dependent.
- Continuation of coverage may only be made available to individuals who have been continuously insured for 3 months prior to termination or change in marital status. An individual who wishes to continue coverage must request continuation in writing no later than 10 days after the terminating event and pay the required premium on a monthly basis and in advance.
- Coverage must end at the earliest of
- 120 days after continuation of coverage began;
- The period for which the individual made a timely contribution;
- The insured becoming eligible for Medicare; or
- The date on which the policy is terminated, or the group withdraws from the plan, except for replacement.
- Upon termination of continued coverage, an insurer must be offered a conversion policy.
- Continued coverage does not need to include benefits for dental care, vision services, or prescription drug expenses. Coverage may not be continued for individuals eligible for Medicare or full coverage under another group health insurance policy.
- Conversion of Coverage — Every group accident and health insurance policy issued in this state, other than coverage limited to expenses from accidents or specified diseases, must provide insureds under a terminated policy the option to convert their group policy to an individual plan. An individual must apply for conversion no later than 30 days after termination of group coverage.
- A converted policy must provide coverage equal to or greater than the minimum standards established by the Commissioner and contain the statement "the benefits in this policy do not necessarily equal or match those benefits provided in your previous group policy." The initial premium for a conversion policy for the first year and subsequent renewal premiums are determined by individually underwritten standard risks for the age and class of risk and the type and amount of insurance provided.
- Converted policies are prohibited from excluding coverage for pregnancy or other illness or injury on the grounds of a pre-existing condition which either exceeds or equals the waiting period of the original group plan.
- Individuals eligible for Medicare or other group health coverage are not eligible for conversion.
E. Small Group Coverage
1. Small Employer
A small employer is any employer actively engaged in business that, on at least 50% of its working days during the past year, employed at least 2 but no more than 50 eligible employees. In determining the number of eligible employees, companies that are affiliated companies or that are eligible to file a combined tax return are considered one employer.
2. Eligible Employee
An eligible employee means an employee or individual who is a full-time employee (working at least 30 hours a week for an eligible employer) and is qualified to enroll in a health benefit plan.
3. Provisions
The health insurance purchasing group providing health insurance for small employers must offer at least 2 types of plans including one plan providing a choice of deductibles with state-mandated health benefits. They may also offer a health benefit plan not subject to state-mandated benefits that does not contain standard provisions or rights required to be present in a health benefit plan pursuant to law or regulations unrelated to a specific health illness, injury, or condition of the insured, for the provisions as may be determined by rules and regulations of the Commissioner.
Every health benefit plan offered through a health insurance purchasing group must meet the following requirements:
- Be underwritten by a health insurance purchasing group health carrier that is licensed or otherwise regulated under state law and meets all applicable state standards relating to consumer protection;
- Be approved or otherwise permitted to be offered under law;
- Provide full portability of creditable coverage for individuals who remain members of the same health insurance purchasing group, notwithstanding that they change the eligible employer through which they are members; and
- Comply with the provisions of the Arkansas Insurance Code in their sales and solicitation of insurance.
F. Health Maintenance Organizations (HMOs)
A Health Maintenance Organization (HMO) is any organization formed under the laws of Arkansas to provide or arrange for one or more health care plans under a system that causes any part of the risk of health care delivery to be borne by the organization or its providers. No HMO or its representative may cause or knowingly permit the use of advertising, solicitation, or any form of evidence of coverage that is untrue, misleading, or deceptive.
In Arkansas, no person can establish or operate an HMO, nor sell, offer to sell, or solicit offers to purchase in conjunction with an HMO without first obtaining a Certificate of Authority.
The powers of a health maintenance organization (HMO) include, but are not limited to:
- Purchasing, leasing, or building hospitals or other health care facilities, including ancillary equipment;
- Making loans to health care providers or corporations for the purpose of constructing medical facilities and hospitals;
- Furnishing healthcare services through contracted providers;
- Contracting with people to perform marketing, enrollment, and administration duties;
- Offering additional healthcare services, indemnity benefits covering out-of-area emergency services, and indemnity benefits on a point-of-service basis; and
- Contracting with out-of-state providers who are licensed to provide medical care in the provider's jurisdiction.
HMOs must file a notice with the Commissioner when exercising powers. If the Commissioner does not disapprove the HMO's actions within 60 days of filing, the exercise of power is approved.
HMOs that have been in operation for at least 2 years may offer an annual open enrollment period of at least 1 month.
In order to maintain financial stability, prevent adverse selection by prospective enrollees, and avoid unreasonably high charges, an HMO may impose underwriting restrictions, upon approval by the Commissioner. The Commissioner must approve or deny an application for underwriting restrictions within 60 days. HMOs providing services on a group contract basis may limit open enrollment to all members of the group.
HMOs must provide to all enrollees evidence of coverage that must contain a statement of the following information:
- The health care services and the insurance or other benefits to which the enrollee is entitled under the contract;
- Any exclusions or limitations on the services, kinds of services, benefits, or kinds of benefits to be provided, including any deductible or copayment feature and requirements for referrals prior to authorizations and second opinions;
- Where and how enrollees can get information about services;
- The total amount of payment and copayment, if any, for health care services and the indemnity or service benefits, if any, that the enrollee is obligated to pay with respect to individual contracts; and
- A description of the HMO's method for resolving enrollee complaints.
G. COBRA Health - State Continuation
Every group accident and health insurance policy providing hospital, surgical, or major medical coverage, other than accident only or specified disease policies, must contain a provision that any certificate holder, member, or spouse whose coverage under the policy would otherwise end due to termination of employment or membership or change in marital status may continue coverage for themselves and their eligible dependents. The continued coverage does not need to include benefits for dental care, vision services, or prescription drug expenses.
Continuation of coverage is available only to individuals who have been insured continuously under the group policy in the 3 months before the event that terminated coverage. Continuation is not available to people eligible for Medicare coverage or full coverage under any other group accident and health policy or contract.
This coverage must provide benefits for all pre-existing conditions to be considered full coverage. Accordingly, an individual may continue his or her previous group coverage until all pre-existing conditions are covered or would be covered under another group policy or contract, or until termination of coverage.
Individuals must request continuation of coverage in writing no later than 10 days after the event that terminated coverage, and must pay the premium required by the policyholder on a monthly basis and in advance.
Continuation of coverage will end upon the earliest of the following dates:
- 120 days after continuation of coverage began;
- The end of the period for which the individual made a timely contribution (paid the policy premium);
- The premium due date following the date the individual becomes eligible for Medicare; or
- The date on which the policy is terminated or the group withdraws from the plan. (If the group policy is replaced, continuation will continue under the new coverage.)
At the termination of the continued coverage, an individual will be offered the conversion policy under the group policy. Individuals who convert the group policy will waive their right to continuation of coverage.
These rules do not apply to health care plans in which the employer is self-insured.
H. Chapter Recap
This chapter focused on state-specific regulations pertaining to health insurance products. Let's recap some of the important provisions that apply to individual and group health policies.
POLICY PROVISIONS
Required Provisions
- Entire contract/changes: a copy of the application must be attached to the policy; changes must be approved by an executive officer of the insurer.
- Time limit on certain defenses: 3 years
- Grace period:
- 7 days for weekly premiums
- 10 days for monthly premiums
- 31 days for any other premium mode
- Reinstatement: immediate coverage for accidents; 10-day waiting period for sickness
- Notice of claim: 20 days
- Claim forms: insurer furnishes within 15 days of notice of claim
- Proof of loss: written proof within 90 days after the end of the period for which the insurer is liable
- Payment of claims: immediately upon receipt of written proof of death
- Legal action: after 60 days but not later than 3 years after proof of loss
Mandatory Coverages
- Newborn children of the insured: covered from birth; insured must notify the insurance company of birth within 90 days
- Mental health services
- Maternity benefits:
- 48 hours for vaginal delivery; 96 hours for cesarean section
- Chiropractic services
- Substance abuse:
- $6,000 for each 24-month period; $12,000 lifetime minimum
MEDICARE SUPPLEMENT POLICIES
Requirements
- Must adhere to NAIC standardized model Medicare supplement policies
- Cannot duplicate Medicare benefits
- Pre-existing condition exclusion: no longer than 6 months
LONG-TERM CARE
Basics
- Any policy or rider designed to provide coverage for at least 12 consecutive months
- Pre-existing condition exclusion: no longer than 6 months
- Must be guaranteed renewable
GROUP/BLANKET COVERAGE
Eligible for Blanket Coverage
- Common carriers, covering all passengers of the common carrier
- Policies issued to any employer
- Institutions of learning, covering students and teachers
- Religious, charitable, recreational, educational, or civic organizations
- Volunteer fire departments or similar volunteer groups
- Sports teams or camps
SMALL GROUP COVERAGE
Small Employer
- Employed at least 2 but no more than 50 eligible employees on at least 50% of working days during the past year
- Eligible employee: full-time, qualified to enroll in health plan
- Must offer at least 2 types of plan
Medicare ID Card
Arkansas Medicare Agent
Meet Rachael Kathleen Rawlins, your knowledgeable and pleasant insurance agent with expertise in saving you time and money, finding the most comprehensive Medicare Plan for you.
Call your Medicare Agent, Rachael Kathleen Rawlins, now.
501-393-2414 or easily enroll here online.
I am Rachael Kathleen Rawlins and I serve all of these Arkansas counties to find you the most savings in your Medicare Plan or Medicare Advantage Plan.
Arkansas, Ashley, Baxter, Benton, Boone, Bradley, Calhoun, Carroll, Chicot, Clark, Clay, Cleburne,
Cleveland, Columbia, Conway, Craighead, Crawford, Crittenden, Cross, Dallas, Desha, Drew,
Faulkner, Franklin, Fulton, Garland, Grant, Greene, Hempstead, Hot Spring, Howard,
Independence, Izard, Jackson, Jefferson, Johnson, Lafayette, Lawrence, Lee, Lincoln, Little River,
Logan, Lonoke, Madison, Marion, Miller, Mississippi, Monroe, Montgomery, Nevada, Newton,
Ouachita, Perry, Phillips, Pike, Poinsett, Polk, Pope, Prairie, Pulaski, Randolph, Saline, Scott,
Searcy, Sebastian, Sevier, Sharp, St. Francis, Stone, Union, Van Buren, Washington, White,
Woodruff and Yell counties
Missouri Medicare Agent
Meet Rachael Kathleen Rawlins, your knowledgeable and pleasant insurance agent with expertise in saving you time and money, finding the most comprehensive Medicare Plan for you.
Call your Medicare Agent, Rachael Kathleen Rawlins, now.
501-393-2414 or easily enroll here online.
I am Rachael Kathleen Rawlins and I serve all of these Missouri counties to find you the most savings in your Medicare Plan or Medicare Advantage Plan.
Missouri Counties and Regions
Part 1: Sorted by Region Showing Region Codes and Counties
| Region Code | Region Name | Counties |
|---|---|---|
| 110 | St. Louis MSA | Franklin, Jefferson, Lincoln, St. Charles, St. Louis, Warren, St. Louis city |
| 203 | Kansas City MSA | Cass, Clay, Clinton, Jackson, Lafayette, Platte, Ray |
| 213 | Springfield - Branson | Christian, Dallas, Greene, Polk, Stone, Taney, Webster |
| 302 | Central | Audrain, Boone, Callaway, Cole, Cooper, Gasconade, Howard, Moniteau, Montgomery, Osage, Randolph |
| 401 | Bootheel | Butler, Carter, Dunklin, Mississippi, New Madrid, Pemiscot, Ripley, Scott, Stoddard, Wayne |
| 404 | Lake Ozark Rolla | Camden, Crawford, Dent, Laclede, Maries, Miller, Morgan, Phelps, Pulaski |
| 405 | Lower East Central-Cape | Bollinger, Cape Girardeau, Iron, Madison, Perry, Reynolds, Ste. Genevieve, St. Francois, Washington |
| 406 | North Central | Carroll, Chariton, Grundy, Linn, Livingston, Mercer, Putnam, Sullivan |
| 407 | Northeast | Adair, Clark, Knox, Lewis, Macon, Marion, Monroe, Pike, Ralls, Schuyler, Scotland, Shelby |
| 408 | Northwest | Andrew, Atchison, Buchanan, Caldwell, Daviess, DeKalb, Gentry, Harrison, Holt, Nodaway, Worth |
| 411 | South Central | Douglas, Howell, Oregon, Ozark, Shannon, Texas, Wright |
| 412 | Southwest | Barry, Barton, Cedar, Dade, Jasper, Lawrence, McDonald, Newton, Vernon |
| 414 | West Central | Bates, Benton, Henry, Hickory, Johnson, Pettis, St. Clair, Saline |
Part 2: Sorted by County
| Fipco | county | Region |
|---|---|---|
| 29001 | Adair | Northeast |
| 29003 | Andrew | Northwest |
| 29005 | Atchison | Northwest |
| 29007 | Audrain | Central |
| 29009 | Barry | Southwest |
| 29011 | Barton | Southwest |
| 29013 | Bates | West Central |
| 29015 | Benton | West Central |
| 29017 | Bollinger | Lower East Central-Cape |
| 29019 | Boone | Central |
| 29021 | Buchanan | Northwest |
| 29023 | Butler | Bootheel |
| 29025 | Caldwell | Northwest |
| 29027 | Callaway | Central |
| 29029 | Camden | Lake Ozark Rolla |
| 29031 | Cape Girardeau | Lower East Central-Cape |
| 29033 | Carroll | North Central |
| 29035 | Carter | Bootheel |
| 29037 | Cass | Kansas City MSA |
| 29039 | Cedar | Southwest |
| 29041 | Chariton | North Central |
| 29043 | Christian | Springfield - Branson |
| 29045 | Clark | Northeast |
| 29047 | Clay | Kansas City MSA |
| 29049 | Clinton | Kansas City MSA |
| 29051 | Cole | Central |
| 29053 | Cooper | Central |
| 29055 | Crawford | Lake Ozark Rolla |
| 29057 | Dade | Southwest |
| 29059 | Dallas | Springfield - Branson |
| 29061 | Daviess | Northwest |
| 29063 | DeKalb | Northwest |
| 29065 | Dent | Lake Ozark Rolla |
| 29067 | Douglas | South Central |
| 29069 | Dunklin | Bootheel |
| 29071 | Franklin | St. Louis MSA |
| 29073 | Gasconade | Central |
| 29075 | Gentry | Northwest |
| 29077 | Greene | Springfield - Branson |
| 29079 | Grundy | North Central |
| 29081 | Harrison | Northwest |
| 29083 | Henry | West Central |
| 29085 | Hickory | West Central |
| 29087 | Holt | Northwest |
| 29089 | Howard | Central |
| 29091 | Howell | South Central |
| 29093 | Iron | Lower East Central-Cape |
| 29095 | Jackson | Kansas City MSA |
| 29097 | Jasper | Southwest |
| 29099 | Jefferson | St. Louis MSA |
| 29101 | Johnson | West Central |
| 29103 | Knox | Northeast |
| 29105 | Laclede | Lake Ozark Rolla |
| 29107 | Lafayette | Kansas City MSA |
| 29109 | Lawrence | Southwest |
| 29111 | Lewis | Northeast |
| 29113 | Lincoln | St. Louis MSA |
| 29115 | Linn | North Central |
| 29117 | Livingston | North Central |
| 29119 | McDonald | Southwest |
| 29121 | Macon | Northeast |
| 29123 | Madison | Lower East Central-Cape |
| 29125 | Maries | Lake Ozark Rolla |
| 29127 | Marion | Northeast |
| 29129 | Mercer | North Central |
| 29131 | Miller | Lake Ozark Rolla |
| 29133 | Mississippi | Bootheel |
| 29135 | Moniteau | Central |
| 29137 | Monroe | Northeast |
| 29139 | Montgomery | Central |
| 29141 | Morgan | Lake Ozark Rolla |
| 29143 | New Madrid | Bootheel |
| 29145 | Newton | Southwest |
| 29147 | Nodaway | Northwest |
| 29149 | Oregon | South Central |
| 29151 | Osage | Central |
| 29153 | Ozark | South Central |
| 29155 | Pemiscot | Bootheel |
| 29157 | Perry | Lower East Central-Cape |
| 29159 | Pettis | West Central |
| 29161 | Phelps | Lake Ozark Rolla |
| 29163 | Pike | Northeast |
| 29165 | Platte | Kansas City MSA |
| 29167 | Polk | Springfield - Branson |
| 29169 | Pulaski | Lake Ozark Rolla |
| 29171 | Putnam | North Central |
| 29173 | Ralls | Northeast |
| 29175 | Randolph | Central |
| 29177 | Ray | Kansas City MSA |
| 29179 | Reynolds | Lower East Central-Cape |
| 29181 | Ripley | Bootheel |
| 29183 | St. Charles | St. Louis MSA |
| 29185 | St. Clair | West Central |
| 29186 | Ste. Genevieve | Lower East Central-Cape |
| 29187 | St. Francois | Lower East Central-Cape |
| 29189 | St. Louis | St. Louis MSA |
| 29195 | Saline | West Central |
| 29197 | Schuyler | Northeast |
| 29199 | Scotland | Northeast |
| 29201 | Scott | Bootheel |
| 29203 | Shannon | South Central |
| 29205 | Shelby | Northeast |
| 29207 | Stoddard | Bootheel |
| 29209 | Stone | Springfield - Branson |
| 29211 | Sullivan | North Central |
| 29213 | Taney | Springfield - Branson |
| 29215 | Texas | South Central |
| 29217 | Vernon | Southwest |
| 29219 | Warren | St. Louis MSA |
| 29221 | Washington | Lower East Central-Cape |
| 29223 | Wayne | Bootheel |
| 29225 | Webster | Springfield - Branson |
| 29227 | Worth | Northwest |
| 29229 | Wright | South Central |
| 29510 | St. Louis city | St. Louis MSA |